What Happens After Egg Transfer in IVF: Your Complete Guide to the Journey Ahead
So, you’ve made it through the egg retrieval and embryo transfer stages of in vitro fertilization (IVF). Congratulations—that’s no small feat! Now, you’re probably wondering: what happens next? The time after the embryo transfer can feel like a rollercoaster of hope, nerves, and questions. Will it work? What should I do—or not do? How will I know if I’m pregnant? If you’re feeling a mix of excitement and uncertainty, you’re not alone. This phase, often called the “two-week wait,” is a big deal for anyone going through IVF, and it’s totally normal to want all the details.
In this guide, we’re diving deep into what happens after the embryo transfer—everything from how your body might respond to what’s going on with that tiny embryo inside you. We’ll cover the science, the emotions, and the practical stuff you can do (or avoid) to feel more in control. Plus, we’ll explore some fresh angles that don’t always get the spotlight, like how your mindset can play a role, what the latest research says about success rates, and even how your partner can support you through this. Whether it’s your first IVF cycle or you’re a seasoned pro, this article is here to give you clarity, hope, and a few surprises along the way. Let’s get started!
The Two-Week Wait: What’s Happening Inside You?
The embryo transfer is done, and now you’re in the infamous two-week wait (TWW)—the stretch of time between the transfer and when you can take a pregnancy test. It’s about 10-14 days, depending on whether you had a day-3 or day-5 embryo transfer. So, what’s going on in there?
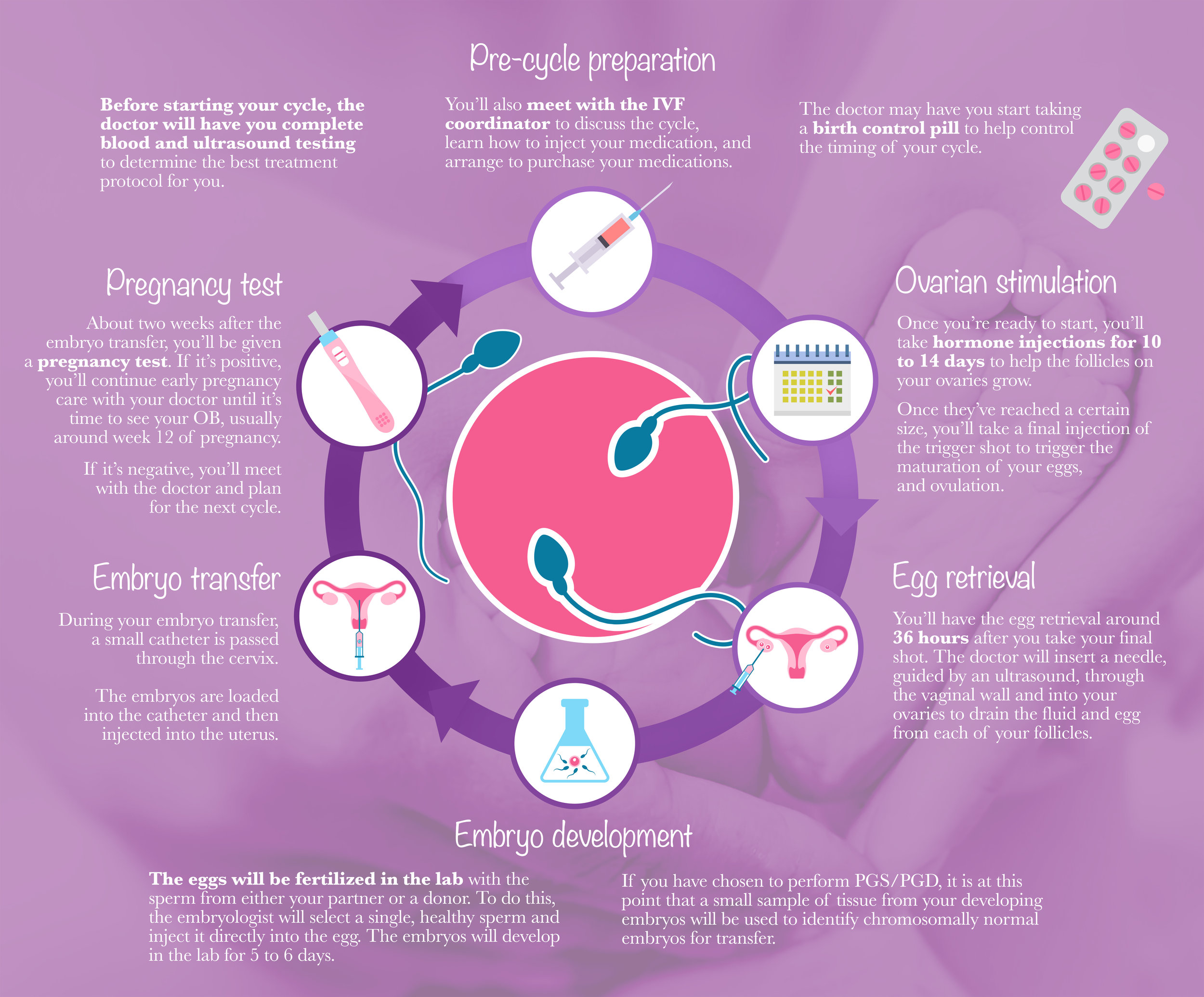
After the doctor places the embryo in your uterus, it doesn’t just sit there—it’s got work to do! The embryo needs to hatch out of its protective shell (called the zona pellucida) and implant into the lining of your uterus. This process, called implantation, is where the magic happens—or doesn’t. Here’s a quick breakdown of the timeline:
- Day 1-2 Post-Transfer: The embryo is floating around in your uterus, getting comfy. If it’s a blastocyst (a day-5 embryo), it might already be starting to hatch.
- Day 3-5: The embryo hatches fully and begins to burrow into the uterine lining. Tiny cells called trophoblasts reach out like little hands, connecting to your blood supply.
- Day 6-10: If implantation works, the embryo starts releasing human chorionic gonadotropin (hCG)—the hormone that pregnancy tests detect. This is when your body might begin to signal, “Hey, something’s happening!”
Sounds simple, right? But here’s the catch: implantation isn’t guaranteed. Studies show that even with a perfect embryo and a healthy uterus, the success rate hovers around 50-60% per transfer for women under 35, dropping as age goes up. Why? It’s a mix of embryo quality, uterine receptivity, and a sprinkle of luck.
What You Might Feel (Or Not Feel)
Your body might give you some clues—or it might stay totally silent. Some people notice mild cramping, spotting, or bloating, which could be implantation or just side effects from the progesterone meds you’re likely taking. Others feel nothing at all and still get a positive test. Don’t panic if you’re symptom-free—it doesn’t mean it didn’t work!
Fresh vs. Frozen Embryo Transfers: Does It Change What Happens?
Not all embryo transfers are the same. You might have had a fresh embryo transfer (right after egg retrieval) or a frozen embryo transfer (FET) from a previous cycle. Does it make a difference? Yep, and here’s how.
Fresh Embryo Transfers
With a fresh transfer, your body’s been through a lot—ovarian stimulation, egg retrieval, and now the transfer. Your hormone levels (like estrogen and progesterone) are sky-high, which can make your uterus super receptive—or sometimes a little overwhelmed. Research from 2023 shows that fresh transfers might have a slightly lower implantation rate (around 5-10% less) compared to FETs for some women, especially if your body overreacted to the stimulation meds, a condition called ovarian hyperstimulation syndrome (OHSS).
Frozen Embryo Transfers
FETs give your body a break. After freezing the embryos, your doctor can time the transfer to match your natural cycle or use meds to prep your uterus. A 2024 study in Fertility and Sterility found that FETs often have higher success rates (up to 65% for women under 35) because the uterus gets a fresh start, free from the hormonal chaos of stimulation. Plus, freezing lets embryologists pick the strongest survivors.
Which Is Better for You?
It depends! Fresh transfers might be faster, but FETs could offer a better shot if your body needs time to reset. Talk to your doctor about your cycle history—they’ll have the scoop on what’s best for you.
Implantation: The Make-or-Break Moment
Implantation is the star of the show after the transfer. It’s when the embryo officially becomes part of you, linking up with your blood supply to grow. But what makes it stick—or slip?
The Science Behind It
Picture this: the embryo is like a seed, and your uterine lining is the soil. For the seed to take root, the soil needs to be just right—soft, thick, and full of nutrients. That’s where progesterone comes in, thickening your lining to create a cozy landing spot. Meanwhile, the embryo’s quality matters too. A 2023 study from the Journal of Assisted Reproduction and Genetics found that blastocysts with higher cell counts and less fragmentation implant better—think of it like choosing a sturdy seedling over a wilted one.
What Can Go Wrong?
Sometimes, the timing’s off. If the embryo and uterus aren’t in sync (called the “window of implantation”), it’s like trying to plant a seed in frozen ground—it won’t take. Other times, genetic issues in the embryo or inflammation in the uterus can throw a wrench in things. That’s why some clinics now use endometrial receptivity tests (like ERA) to pinpoint the perfect moment.
Signs of Implantation
- ✔️ Light spotting (implantation bleeding) 6-12 days after transfer
- ✔️ Mild cramps that feel like period twinges
- ❌ Heavy bleeding or severe pain (call your doctor if this happens!)
The Emotional Ride: Coping with the Wait
Let’s be real: the two-week wait can mess with your head. One minute you’re googling “early pregnancy signs,” and the next you’re convinced it didn’t work because you sneezed too hard. Sound familiar? Here’s how to keep your sanity.
Why It’s So Hard
Your brain’s wired to fill in blanks, especially when the stakes are high. A 2024 survey by the American Society for Reproductive Medicine found that 78% of IVF patients rank the TWW as the toughest part—more than injections or retrieval. The uncertainty is brutal, but you’ve got this.
Tips to Stay Grounded
- Distract Yourself: Binge a silly show, bake cookies, or finally organize that closet. Keep your hands and mind busy.
- Lean on Your Crew: Tell your partner, bestie, or an IVF support group how you’re feeling. They can’t fix it, but they can listen.
- Skip the Early Test: Testing too soon (before day 9-11) can give false negatives and crush your vibe. Hold off for the blood test if you can.
Mini Quiz: How Are You Holding Up?
Take a sec to check in with yourself:
- Are you sleeping okay, or is your brain on overdrive?
- Do you feel hopeful, anxious, or a wild mix of both?
- Have you found something fun to do today?
No right answers—just a nudge to see where you’re at. If it’s rough, give yourself grace. This isn’t easy.
Your Body on Progesterone: What’s Normal?
After the transfer, you’re probably taking progesterone—pills, shots, or suppositories—to support your uterine lining. It’s a game-changer, but it comes with side effects that can trick you into thinking you’re pregnant (or not).
What It Does
Progesterone keeps your uterus plush and ready for implantation. Without it, the lining might shed, and the embryo wouldn’t stand a chance. Studies show it boosts success rates by 10-15% in IVF cycles.
What You Might Notice
- ✔️ Bloating that makes your jeans feel tight
- ✔️ Sore breasts (thanks, hormones!)
- ✔️ Fatigue that hits like a truck
- ❌ Mood swings that rival a soap opera
These mimic early pregnancy, so don’t read too much into them. They’re just progesterone doing its job.
Pro Tip
If shots are your thing, warm the oil with your hands first—it stings less. And if suppositories are messy, use a panty liner. Small tweaks, big relief.
The Pregnancy Test: When and What to Expect
The big moment’s coming: the pregnancy test. Your clinic will likely schedule a blood test 9-14 days post-transfer to measure hCG. Here’s the lowdown.
Timing Matters
- Day-5 Transfer: Test around day 9-11.
- Day-3 Transfer: Wait until day 11-14.
Why? hCG needs time to build up. Test too early, and you might miss it.
What the Numbers Mean
- <5 mIU/mL: Not pregnant (sorry, friend).
- 5-25 mIU/mL: Gray area—might be too early or a chemical pregnancy.
- >25 mIU/mL: Positive! Your clinic will retest in 48 hours to see if it doubles (a good sign).
Home Tests: Yay or Nay?
Tempted to pee on a stick? Home tests can work but aren’t as sensitive as blood tests. Plus, fertility meds can cause false positives. If you can’t resist, wait until at least day 10 and brace for mixed both results.
If It Works: Next Steps
Positive test? Woo-hoo! Here’s what’s next.
Early Pregnancy Monitoring
Your clinic will track your hCG levels and schedule an ultrasound around 6-7 weeks to check for a heartbeat. Rest up—your body’s working overtime now.
What to Watch For
- ✔️ Light spotting is okay in the first trimester.
- ❌ Heavy bleeding or sharp pain? Call your doctor ASAP.
Fun Fact
Did you know twins are more common with IVF (about 20-30% of pregnancies)? If you transferred two embryos, you might get double the joy!
If It Doesn’t Work: You’re Still Enough
A negative test stinks—no sugarcoating it. It’s okay to cry, scream, or eat a whole pint of ice cream. But here’s the truth: this isn’t the end of your story.
Why It Might Happen
- Embryo issues (genetic glitches are common)
- Uterine factors (lining or timing off)
- Plain old chance (IVF isn’t 100%)
Moving Forward
Take time to heal—emotionally and physically. Then, chat with your doctor. A 2024 study showed that 65% of women who try another cycle after a failure eventually succeed. You’ve got options: another transfer, a new approach, or even a break.
A Little Perspective
One woman I heard about had three failed transfers before switching to a new protocol—and now she’s got a toddler. It’s not over until you say it is.
Beyond the Basics: 3 Things You Haven’t Heard Enough About
Most articles stop at the test, but let’s go deeper. Here are three topics that deserve more airtime.
1. The Gut-Implantation Connection
Your gut health might affect IVF success—crazy, right? A 2023 study in Microbiome found that women with balanced gut bacteria had higher implantation rates. How? A healthy microbiome reduces inflammation, which can make your uterus more welcoming. Try adding yogurt, kefir, or a probiotic to your routine (check with your doc first!).
2. Your Partner’s Role Post-Transfer
Partners often feel sidelined in IVF, but they’re key during the TWW. Ask them to handle chores, cook a cozy meal, or just hold you when you’re freaking out. A 2024 survey found that couples who shared the emotional load reported less stress and stronger bonds.
3. Mindset and Success Rates
Can positive thinking boost your odds? Maybe! A 2023 study in Human Reproduction showed that women with lower stress levels pre- and post-transfer had a 10% higher success rate. Meditation, journaling, or even laughing at a dumb movie could tip the scales.
Your IVF Survival Kit: Practical Tips for the Wait
Here’s a cheat sheet to make the TWW smoother:
- Do This:
- Eat balanced meals (protein + veggies = happy hormones).
- Walk or stretch gently—keeps blood flowing without overdoing it.
- Set a daily “worry window” (15 mins to freak out, then move on).
- Skip This:
- Heavy lifting or intense workouts (give your body a break).
- Googling every twinge (it’s a rabbit hole of stress).
- Caffeine overload (a little’s fine, but don’t chug espresso).
Poll: What’s Your Go-To Distraction?
What keeps you sane during the wait? Vote below and see what others say!
- Binge-watching Netflix
- Crafting or DIY projects
- Chatting with friends
- Napping (because why not?)
Check back next week for the results!







