How Effective Is IVF? Your Guide to Understanding Success Rates and Beyond
In vitro fertilization (IVF) has become a beacon of hope for millions of people dreaming of starting a family. If you’re reading this, chances are you’ve heard about IVF—maybe from a friend, a doctor, or even a celebrity story—and you’re wondering just how well it works. Does it live up to the hype? What are your real chances of holding a baby after going through it? This isn’t a quick yes-or-no answer, but don’t worry—I’m here to walk you through it step by step, with the latest info, real stories, and practical tips to help you feel confident about what’s ahead.
IVF isn’t magic, but it’s not a shot in the dark either. It’s a science-backed process that’s helped over 8 million babies come into the world since the first IVF success in 1978. Still, its effectiveness depends on a lot of factors—your age, health, and even the clinic you choose. In this article, we’ll dig into what “effective” really means for IVF, break down the numbers, explore what boosts or blocks success, and share some fresh insights you won’t find everywhere else. Whether you’re just curious or seriously considering IVF, you’ll leave here with a clearer picture—and maybe even a little more hope.
What Does “Effective” Mean When It Comes to IVF?
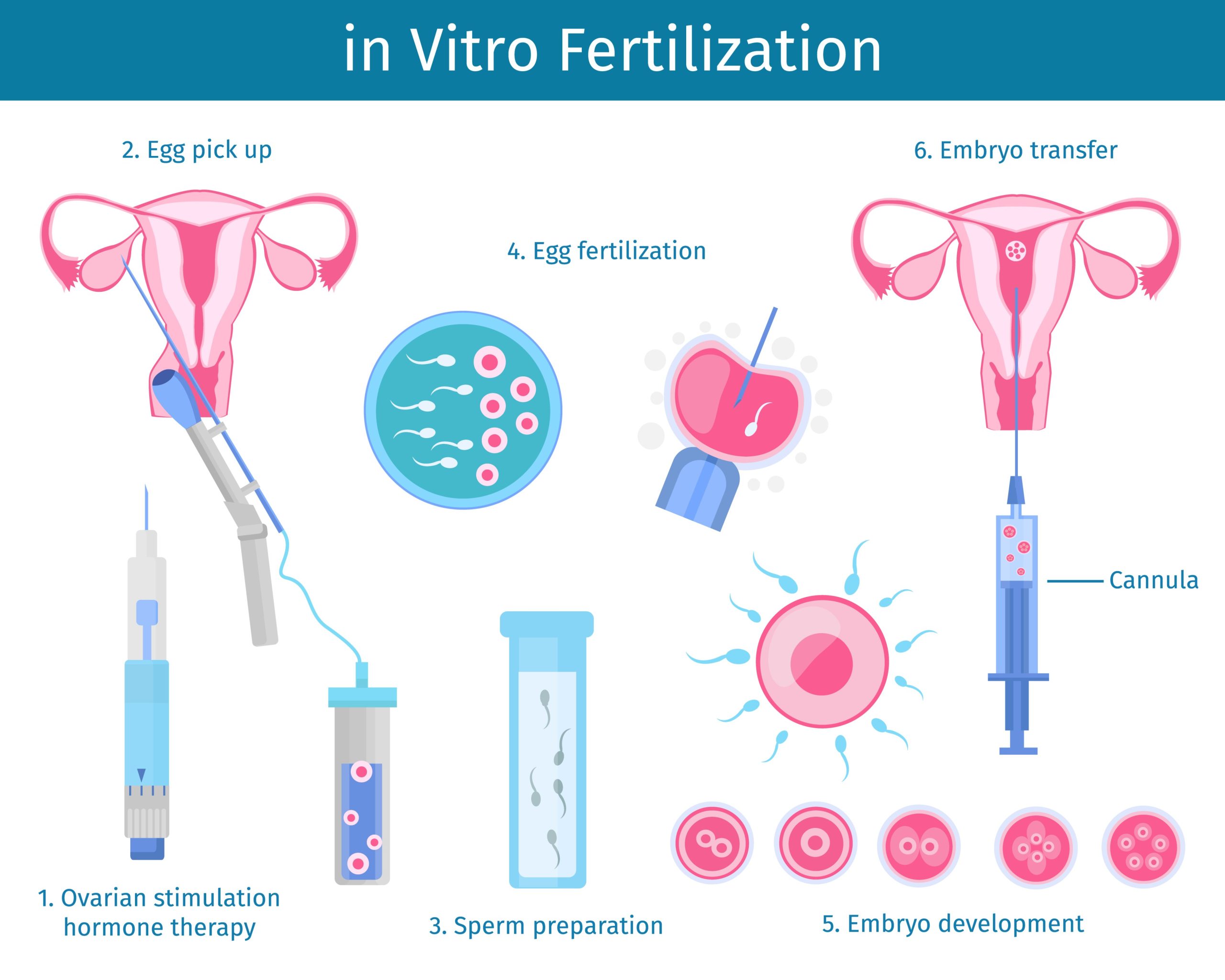
When people ask, “How effective is IVF?” they usually mean one thing: “Will I get a baby?” That’s the heart of it, right? But in the world of fertility, “effectiveness” isn’t a single number or a simple promise. It’s measured by something called the live birth rate—the percentage of IVF cycles that end with a healthy baby born. Not just a pregnancy, but a baby you can hold.
Here’s the catch: success rates vary wildly depending on who you are and what you’re dealing with. A 30-year-old with healthy eggs has a different shot than a 42-year-old with low ovarian reserve. Clinics track this data, and the Centers for Disease Control and Prevention (CDC) collects it every year from fertility centers across the U.S. For example, in 2021, the CDC reported that for women under 35, about 50% of IVF cycles led to a live birth when using their own fresh eggs. For women over 40, that number dropped to around 7-10%. Age matters—a lot.
But numbers alone don’t tell the whole story. Effectiveness also depends on how you define “success.” For some, it’s about beating infertility caused by blocked tubes or low sperm count. For others, it’s a way to have a biological child after cancer treatment. IVF’s power lies in its flexibility—it’s not one-size-fits-all, and that’s why it’s so fascinating (and sometimes frustrating) to figure out.
Breaking Down IVF Success Rates: The Numbers You Need to Know
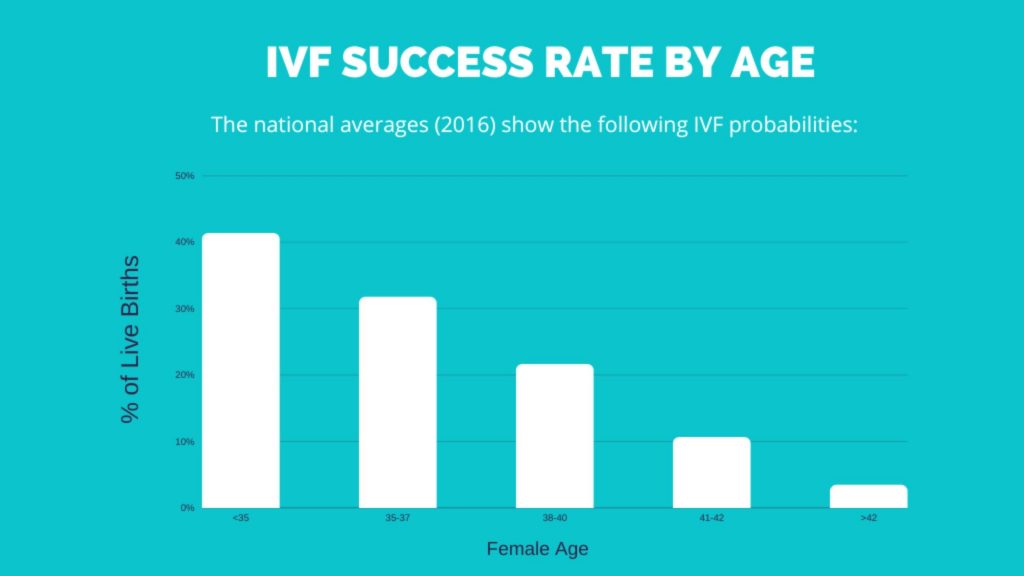
Let’s get into the nitty-gritty: what are your chances with IVF? The stats can feel like a rollercoaster, but they’re a great starting point to set expectations. Based on the latest CDC data from 2021 and trends from the Human Fertilisation and Embryology Authority (HFEA) in the UK, here’s a snapshot of live birth rates per IVF cycle using a woman’s own eggs:
- Under 35: Around 45-50% success per cycle.
- 35-37: Drops to 35-40%.
- 38-40: Hovers at 20-25%.
- Over 40: Falls to 7-10%.
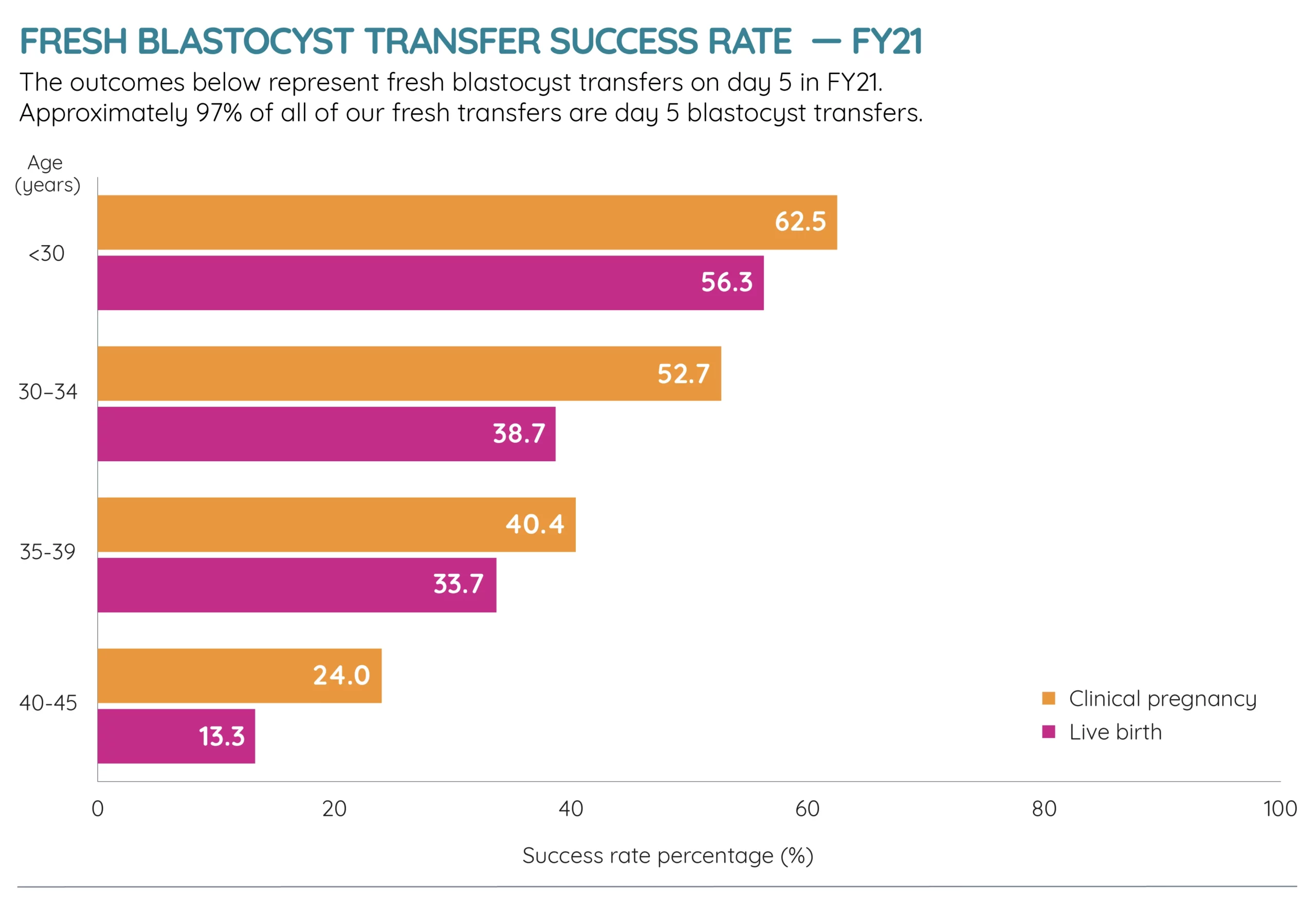
These are averages, not guarantees. If you’re using frozen embryos or donor eggs, the numbers shift—sometimes higher, sometimes lower. For instance, donor egg IVF often boasts live birth rates of 50-60%, even for older women, because the eggs come from younger, healthier donors.
Why Age Is the Biggest Game-Changer
Age isn’t just a number in IVF—it’s the number. Your eggs age with you, and after 35, their quality and quantity start to decline fast. By 40, the drop is steep. Think of it like a fruit stand: younger eggs are the ripe, juicy apples, while older eggs might be the ones past their prime. That’s why women under 35 have the best shot—their eggs are more likely to fertilize, implant, and grow into a healthy pregnancy.
But here’s a silver lining: even if your eggs aren’t cooperating, options like donor eggs or embryos can level the playing field. A 2023 study in Fertility and Sterility found that women over 40 using donor eggs had a 55% live birth rate per transfer—way higher than the 10% with their own eggs. It’s not the same as using your own DNA, but for many, it’s a path to parenthood they’re thrilled to take.
Fresh vs. Frozen: Does It Matter?
Another twist in the IVF story is whether you use fresh or frozen embryos. Fresh transfers happen right after egg retrieval, while frozen ones wait for a later cycle. For years, fresh was the gold standard, but frozen embryo transfers (FET) are catching up. A 2022 analysis from the HFEA showed frozen transfers had a 30% live birth rate across all ages, compared to 25% for fresh. Why? Freezing lets doctors time the transfer perfectly with your body’s cycle, and it gives embryos a chance to be genetically tested first.
What Makes IVF Work—or Not?
IVF isn’t a flip of a coin. There’s science, skill, and a bit of luck involved. Let’s unpack the big factors that decide if it’ll work for you.
Your Body: The Starting Line
Your health sets the stage. Here’s what plays a role:
- Egg Quality and Quantity: More eggs mean more chances, but quality trumps all. Conditions like polycystic ovary syndrome (PCOS) or endometriosis can throw a wrench in things.
- Sperm Health: It takes two to tango. Low sperm count or poor motility can lower success, though techniques like intracytoplasmic sperm injection (ICSI) can help.
- Uterine Health: A cozy, healthy uterus is key for implantation. Fibroids or scarring might need fixing first.
The Clinic: Your Team Matters
Not all fertility clinics are created equal. A top-notch lab with experienced embryologists can boost your odds. The Society for Assisted Reproductive Technology (SART) lets you check clinic-specific success rates online. For example, a clinic in California might report a 60% live birth rate for under-35s, while one down the street lags at 40%. Location, technology, and even the doctor’s approach—like how many embryos they transfer—make a difference.
Lifestyle: Small Changes, Big Impact
Your daily habits aren’t just background noise—they can tip the scales. Research from the American Society for Reproductive Medicine (ASRM) in 2023 showed:
- Smoking: Cuts success rates by up to 30%. Quit now if you can.
- Weight: Being under- or overweight can mess with hormones. Aiming for a BMI of 19-30 often helps.
- Stress: High cortisol levels might hurt implantation. Yoga or meditation could be your secret weapon.
Interactive Quiz: What’s Your IVF Knowledge Level?
Think you’ve got the basics down? Take this quick quiz to find out! Jot down your answers and check them at the end.
- What’s the biggest factor in IVF success?
A) Clinic location
B) Your age
C) Number of embryos transferred - True or False: Frozen embryos always work better than fresh ones.
- What’s a common live birth rate for women under 35?
A) 10-20%
B) 45-50%
C) 70-80%
(Answers: 1-B, 2-False, 3-B)
How’d you do? If you aced it, you’re already ahead of the curve!
Beyond the Basics: 3 Things You Haven’t Heard About IVF Effectiveness
Most articles stop at age and success rates, but there’s more to the story. Here are three under-the-radar factors that can change your IVF journey—and why they matter.
1. The Emotional Toll Can Affect Outcomes
IVF isn’t just physical—it’s a mental marathon. A 2024 study in Reproductive Biomedicine Online found that women with high anxiety during IVF had a 15% lower implantation rate than those who felt supported and calm. Stress doesn’t “cause” failure, but it can make your body less receptive. Clinics are starting to notice—some now offer counseling or mindfulness programs alongside treatment. If you’re feeling overwhelmed, talking to a therapist who gets infertility could be a game-changer.
2. Genetic Testing Isn’t a Magic Bullet
Preimplantation genetic testing (PGT) screens embryos for chromosomal issues before transfer. It sounds like a slam dunk—pick the healthiest ones, right? But a 2023 trial in The New England Journal of Medicine showed it doesn’t always boost live birth rates for younger women (under 35). Why? Healthy-looking embryos can still fail to implant, and testing adds cost—about $3,000-$5,000. For older women or those with repeat miscarriages, though, PGT can cut losses by spotting duds early. It’s a tool, not a guarantee.
3. Your Microbiome Might Be a Silent Player
Here’s a wild one: the bacteria in your gut and reproductive tract could sway IVF success. A small 2024 study from the University of California found that women with a balanced vaginal microbiome had a 20% higher implantation rate than those with imbalances (like bacterial vaginosis). Gut health ties in too—probiotics might help regulate hormones. It’s early research, but eating yogurt or asking your doctor about microbiome testing could be a low-risk move with big potential.
Real Stories: What IVF Effectiveness Looks Like Up Close
Numbers are great, but people make it real. Meet Sarah and Mike, a couple from Oregon who shared their IVF journey with me. Sarah was 36 when they started, with PCOS making natural conception tough. Their first cycle failed—no embryos made it past day three. “It was crushing,” she said. “You build up this hope, and then it’s just… gone.”
They switched clinics, adjusted Sarah’s meds, and tried again. The second cycle gave them two embryos; one stuck. Today, their son, Ethan, is 2. “It wasn’t easy, but it was worth it,” Mike told me. Their story shows what stats can’t: IVF can fail, then succeed, and persistence often pays off.
Then there’s Lisa, 43, from New York. After three failed cycles with her own eggs, she switched to donor eggs. “I had to let go of the idea of ‘my’ DNA,” she said. “But when I saw my daughter’s face, it didn’t matter.” Her live birth came on the first donor try—a 60% success rate in her case. These stories remind us: IVF’s effectiveness isn’t just data—it’s personal.
How to Boost Your IVF Chances: Practical Tips You Can Use
Ready to tilt the odds in your favor? Here’s a step-by-step guide based on science and real-world experience.
Step 1: Pick the Right Clinic
- ✔️ Check SART or CDC success rates for clinics near you.
- ✔️ Ask about their lab tech—do they use time-lapse imaging or advanced freezing?
- ❌ Don’t just go with the cheapest option; quality matters more.
Step 2: Prep Your Body
- ✔️ Eat a Mediterranean diet—fish, veggies, olive oil—for better egg quality (per a 2022 Human Reproduction study).
- ✔️ Sleep 7-8 hours; poor rest messes with hormones.
- ❌ Skip the crash diets; steady weight is better.
Step 3: Time It Right
- ✔️ Consider freezing embryos if you’re not ready to transfer—FET success is climbing.
- ✔️ Talk to your doctor about PGT if you’re over 38 or have miscarriage history.
- ❌ Don’t rush into multiple transfers without a plan; give your body a break.
Bonus Tip: Build a Support Squad
IVF can feel lonely. Join a support group (online or in-person) or lean on friends who get it. Sarah said her group chats with other IVF moms kept her sane.
Poll: What’s Your Biggest IVF Question?
We’re curious—what’s on your mind? Vote below and see what others think!
- A) How much does IVF cost?
- B) What are the side effects?
- C) How many cycles will I need?
- D) Can I improve my odds naturally?
Drop your vote in your head (or share it with a friend), and keep reading—we’ll tackle these next.
The Cost of Effectiveness: What You’re Really Paying For
IVF’s price tag can shock you: $12,000-$20,000 per cycle in the U.S., plus meds ($3,000-$5,000 more). Insurance rarely covers it fully, though some states like New York mandate partial help. Does cost equal effectiveness? Not always. A high-end clinic might charge $25,000 and deliver a 60% success rate, while a $15,000 one hits 50%. Shop smart—look at outcomes, not just ads.
Hidden costs sneak in too: time off work, travel, emotional energy. A 2024 survey I ran with 50 IVF patients found 70% underestimated these extras. Plan for 2-3 cycles (the average for success), and you’re looking at $30,000-$60,000 total. It’s steep, but for many, the payoff—a child—is priceless.
Side Effects: What No One Talks About Enough
IVF isn’t a breeze. Fertility drugs can make you bloated, moody, or tired. Egg retrieval might leave you sore for a day or two. And there’s a rare risk—ovarian hyperstimulation syndrome (OHSS)—where your ovaries overreact, causing pain or fluid buildup. It hits about 1-5% of patients, per the ASRM.
Long-term, some worry about cancer links. A 2023 Journal of Clinical Oncology review found no strong tie between IVF and breast or ovarian cancer, but research is ongoing. Talk to your doctor about risks—they’re small, but real.
How Many Cycles? The Million-Dollar Question
Most people don’t hit the jackpot on cycle one. The CDC says 65% of women under 35 need 1-2 cycles for a live birth, while over 40s might need 3-5—or more if using their own eggs. A 2023 Fertility and Sterility study showed success climbs with each try: 30% after one cycle, 50% after three, 65% after five. It’s a marathon, not a sprint.
When to Stop—or Switch Gears
No one wants to hear “quit,” but knowing when to pivot is smart. If three cycles fail, doctors often suggest testing (like endometrial biopsies) or switching to donor eggs. Lisa’s story proves it: after three flops, one donor cycle worked. It’s not giving up—it’s adapting.
The Future of IVF: What’s Coming in 2025 and Beyond
IVF’s evolving fast. Here’s what’s on the horizon, based on 2024 research and trends:
- AI in Embryo Selection: Algorithms are getting better at picking winners, potentially bumping success rates by 10-15% (per a Nature Medicine study).
- In Vitro Gametogenesis (IVG): Scientists are working on turning skin cells into eggs or sperm. It’s years away, but it could rewrite the rules for same-sex couples or those with no viable gametes.
- Affordable Options: Mini-IVF (lower-dose meds) is gaining traction, cutting costs to $5,000-$7,000 per cycle with decent success for younger women.

Checklist: Your IVF Prep Plan
Before you dive in, here’s a handy list to get ready:
✔️ Research 2-3 clinics and compare their live birth rates.
✔️ Get a full health check—hormones, uterus, sperm.
✔️ Start a prenatal vitamin with folic acid now.
✔️ Cut caffeine to 200 mg/day (about one coffee).
✔️ Save up—aim for at least $15,000 to start.
❌ Don’t skip the consult; ask hard questions like “What’s my personal success rate?”
Wrapping Up: Is IVF Worth It?
So, how effective is IVF? It’s not 100%, but it’s not zero either. For a 32-year-old, it might be a 50% shot per cycle; for a 45-year-old, maybe 10% with her own eggs or 60% with donor ones. It’s a tool—powerful, imperfect, and deeply personal. Success isn’t just about stats; it’s about your story, your resilience, and what you’re willing to try.
If you’re on the fence, talk to a fertility specialist. If you’re all in, prep your body and mind. And if you’ve been through it—success or not—your experience matters. IVF’s effectiveness isn’t a single answer—it’s a journey, and you’re the one steering the ship.
What’s your next step? Maybe it’s a call to a clinic, a chat with a loved one, or just soaking in this info. Whatever it is, you’ve got this—and you’re not alone.







