How Long Is the IVF Procedure? Your Complete Guide to Timing and What to Expect
In vitro fertilization (IVF) can feel like a big, mysterious journey when you’re first looking into it. If you’re wondering how long the process takes, you’re not alone—it’s one of the most common questions people have when they start exploring fertility treatments. The truth is, IVF isn’t a one-size-fits-all timeline. It’s a series of steps that can stretch over weeks or even months, depending on your body, your doctor’s plan, and a little bit of luck.
In this guide, we’ll walk you through every phase of IVF, break down the time it takes, and dig into details you might not find everywhere else—like how your daily life fits into the schedule, what new research says about timing, and practical tips to make it all less overwhelming. Whether you’re just curious or ready to dive in, here’s everything you need to know about how long IVF really takes.
The Big Picture: How Long Does IVF Take From Start to Finish?
IVF isn’t a single event—it’s a process with multiple stages, each with its own timeline. On average, one full IVF cycle takes about 3 to 6 weeks from the moment you start medications to the day you get a pregnancy test. But that’s just the core cycle. If you zoom out, the entire journey—including prep work, waiting periods, or extra cycles—can span 2 to 6 months or more.
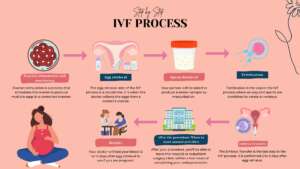
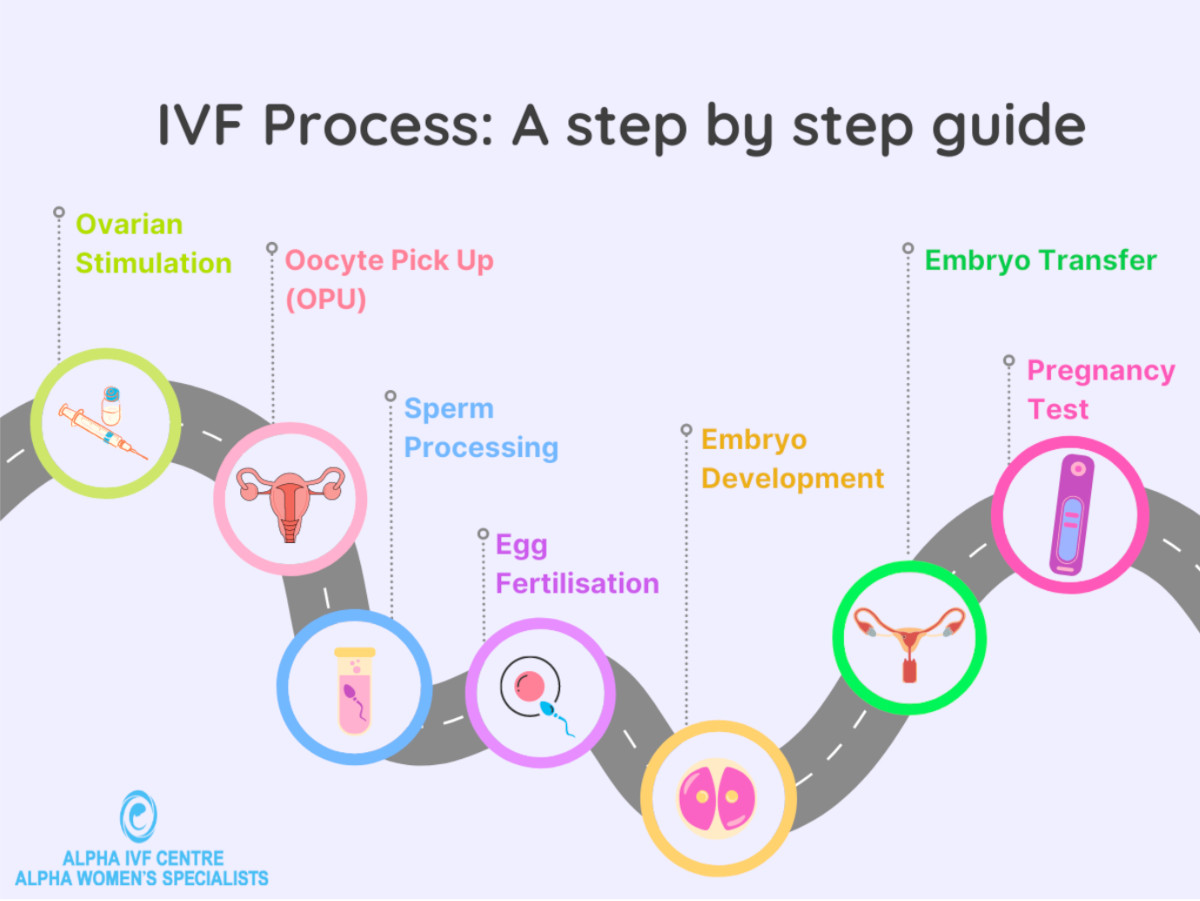
Here’s a quick snapshot of the main phases:
- Prep and Testing: 2-4 weeks (sometimes longer if you need extra steps).
- Ovarian Stimulation: 8-14 days.
- Egg Retrieval: 1 day (about 30 minutes for the procedure itself).
- Fertilization and Embryo Growth: 3-6 days.
- Embryo Transfer: 1 day (a quick 10-15 minute process).
- Waiting for Pregnancy Results: 9-14 days.
That’s the basic rundown, but every step has its own quirks. Let’s dive into each one so you can see how the clock ticks—and what might stretch or shrink the timeline.
Step 1: Getting Ready—What Happens Before the IVF Clock Starts?
Before you even begin the “official” IVF cycle, there’s a prep phase that can take anywhere from 2 to 4 weeks, though it might stretch longer if your situation is unique. This is when your doctor makes sure everything’s lined up for success.
What’s Involved?
You’ll start with a bunch of tests—blood work to check hormone levels, ultrasounds to peek at your ovaries, and maybe a semen analysis if a partner’s involved. Your doctor might also ask about your medical history, lifestyle, and any past pregnancies. It’s like a tune-up for your body to make sure the engine’s ready to roll.
How Long Does It Take?
- Standard Cases: 2-3 weeks. You’ll have appointments spaced out to match your menstrual cycle (usually starting on day 1 or 2 of your period).
- Complex Cases: 4-6 weeks or more. If you’ve got irregular cycles, PCOS, or need surgery (like removing fibroids), this part can drag on.
Pro Tip: Use This Time Wisely
While you’re waiting, tweak your routine to boost your chances. Studies from the American Society for Reproductive Medicine (2023) show that cutting caffeine to under 200 mg a day and getting 7-8 hours of sleep can improve egg quality. Small changes now can pay off later.
Step 2: Ovarian Stimulation—Revving Up Your Ovaries
Once you’re cleared to start, the first big chunk of the IVF cycle kicks off: ovarian stimulation. This usually lasts 8 to 14 days, depending on how your body responds.
What Happens Here?
Your doctor gives you hormone shots (like FSH or HMG) to trick your ovaries into producing multiple eggs instead of the usual one. You’ll visit the clinic every few days for ultrasounds and blood tests to track how those eggs are growing.
Why the Time Varies
- Fast Responders: Some people’s ovaries jump into action, and 8-10 days is enough.
- Slow Starters: If your follicles (the sacs holding the eggs) grow lazily, it might take 12-14 days—or longer if your doctor adjusts the meds.
A Day-in-the-Life Peek
Picture this: You’re giving yourself a shot every evening (don’t worry, the needles are tiny), juggling work, and popping into the clinic every 2-3 days. It’s busy, but doable. One 2024 study from the Journal of Fertility and Sterility found that women who set a consistent injection time (say, 8 PM) had less stress and better hormone consistency. Pick a time and stick to it!
Step 3: Egg Retrieval—The Big Day
After your eggs are ready, it’s time for retrieval. This step takes just 1 day, with the procedure itself lasting about 20-30 minutes.
How It Works
You’ll be under light sedation (think twilight sleep—you’re out but breathing on your own). The doctor uses an ultrasound-guided needle to scoop the eggs from your ovaries through your vagina. It’s quick, but you’ll need a few hours to recover before heading home.
Timing Twist
The exact day depends on your trigger shot—a final injection (usually hCG) given 36 hours before retrieval to ripen the eggs. Miss that window, and the eggs could ovulate on their own, so timing’s tight.
Recovery Reality
Plan to chill for the rest of the day. Most people feel crampy or bloated but bounce back by the next morning. A 2025 survey by FertilityIQ found 80% of patients were back to normal within 24 hours—good news if you’re juggling a busy life.
Step 4: Fertilization and Embryo Growth—Lab Magic
Now the lab takes over. This phase lasts 3 to 6 days, depending on your doctor’s plan.
What’s Happening?
The eggs get mixed with sperm (or injected with it in a process called ICSI). If all goes well, they turn into embryos. The embryologist watches them grow, picking the strongest ones for transfer.
Day 3 vs. Day 5: A Key Choice
- Day 3 Transfer: Embryos are moved to your uterus after 3 days. Faster, but less info on which ones are healthiest.
- Day 5 Transfer: Waiting until day 5 (blastocyst stage) takes longer but boosts success rates—up to 50% for women under 35, per 2024 CDC data.
Hidden Factor: Freezing
Some clinics freeze all embryos after this step and transfer them later. That adds a month or two to the timeline, but research from Yale Medicine (2023) shows frozen transfers can have a 5-10% higher success rate. Worth a chat with your doctor!
Step 5: Embryo Transfer—A Quick but Big Moment
The transfer itself is fast—10-15 minutes—and happens 1 day in the cycle.
The Process
You’re awake, lying on a table. The doctor slides a thin catheter through your cervix to place the embryo(s) in your uterus. It’s like a gentle nudge to get things started—no anesthesia needed.
Fresh vs. Frozen
- Fresh Transfer: Done 3-6 days after retrieval.
- Frozen Transfer: Could be weeks or months later, depending on your body and schedule.
Aftercare Tip
Rest for a few hours, but don’t overdo the bed rest. A 2024 study in Human Reproduction found light activity (like a short walk) after transfer didn’t hurt success rates—and might even help you relax.
Step 6: The Two-Week Wait—Testing Time
Now comes the hardest part: waiting 9-14 days to see if you’re pregnant.
What’s Going On?
Your embryo (hopefully) implants in your uterus, and your body starts making hCG—the pregnancy hormone. A blood test at the clinic confirms the result.
Why the Range?
- Day 3 Transfers: Test around day 12-14.
- Day 5 Transfers: Test as early as day 9-11 since the embryo’s more developed.
Coping Trick: Mini Quiz!
How do you handle the wait? Take this quick quiz:
- A) Binge-watch a new show.
- B) Journal your feelings.
- C) Google every twinge (spoiler: not recommended!).
Pick one and stick to it—distraction is your friend!
What If It Doesn’t Work? Timing the Next Try
If the test is negative, you’ll likely wait 4-6 weeks before starting another cycle—time for your body to reset with a full menstrual cycle. Emotionally, this break can help too. About 60% of people need more than one cycle, per 2023 NIH stats, so don’t lose hope.
Speeding Things Up
Some clinics offer “back-to-back” cycles if you’ve got frozen embryos ready. That cuts the wait to 2-3 weeks. Ask your doctor if this fits your plan.
Beyond One Cycle: The Full IVF Journey
So, how long is IVF really? If you’re lucky and get pregnant on the first try, you’re looking at 2-3 months from prep to positive test. But if you need multiple cycles, factor in:
- Rest Between Cycles: 1-2 months each.
- Frozen Embryo Transfers: Adds 1-2 months per attempt.
- Total Time: Could be 6 months to a year—or more if you pause for health or financial reasons.
A 2025 White House report on IVF access noted that 1 in 7 couples face infertility, and many take 2-3 cycles to succeed. Patience is part of the game.
Unique Angles: What You Won’t Find Everywhere
Most articles stop at the basics, but here are three things you might not know about IVF timing—and why they matter.
1. The Micro-Timing of Your Cycle
Your menstrual cycle’s quirks can shift everything. A 2024 study from PMC found that women with shorter cycles (under 26 days) often finish stimulation faster—by up to 2 days—than those with longer ones. Track your periods for a few months before starting; it could give your doctor a head start.
2. Automation’s Cutting the Clock
New tech is shaking things up. “Lab-on-a-chip” systems, tested in 2023 at UCSF, automate egg and embryo handling, shaving 1-2 days off the lab phase. It’s not everywhere yet, but clinics adopting it could speed your cycle. Ask if your center’s on the cutting edge!
3. The Emotional Timeline
No one talks about this enough, but the mental wait can feel longer than the physical one. A 2025 FertilityIQ poll found 70% of patients said the two-week wait felt “endless” compared to the 6-week prep. Plan mini-goals—like a weekend getaway—to keep your spirits up.
Practical Tips to Navigate the IVF Timeline
Here’s how to make the most of every stage:
✔️ Prep Phase: Stock up on healthy snacks—think nuts and berries—to fuel your body.
✔️ Stimulation: Set phone reminders for shots and appointments; it’s easy to lose track.
✔️ Retrieval Day: Bring a cozy blanket to the clinic—sedation can leave you chilly.
✔️ Transfer: Wear loose pants; tight waistbands can bug you after.
❌ Don’t: Obsess over every symptom post-transfer. It’s normal to feel something—or nothing.
Real-Life Example: Sarah’s Story
Sarah, a 34-year-old teacher, started IVF in January 2025. Her prep took 3 weeks due to a thyroid tweak. Stimulation lasted 10 days, retrieval was a breeze, and she did a day-5 frozen transfer a month later. Her positive test came in April—about 3.5 months total. “The waiting was brutal,” she says, “but breaking it into chunks helped me stay sane.”
How Does Your Age Affect Timing?
Age doesn’t just impact success rates—it can tweak the timeline too. Women over 35 might need longer stimulation (12-14 days vs. 10) because ovaries respond slower, per a 2024 Mayo Clinic report. Younger folks (under 30) often breeze through in 8-10 days. Knowing this can set realistic expectations.
Interactive Poll: What’s Your IVF Pace?
How fast do you want to move? Vote below:
- A) One cycle, quick and done!
- B) Slow and steady, with breaks.
- C) Whatever my doctor says.
Drop your pick in your mind—or share with a friend doing IVF!
Latest Research: What’s Changing IVF Timing?
Science is always tweaking the process. Here’s what’s new in 2025:
- Shorter Protocols: A 2024 NIH trial found “mild stimulation” (fewer drugs, 7-9 days) works for some, cutting time without slashing success.
- AI Predictions: Clinics like Cleveland Clinic are using AI to predict egg growth, trimming monitoring visits by 1-2 days.
- Frozen Future: Freezing all embryos is trending—70% of U.S. cycles in 2024 used it, per CDC, adding flexibility to your schedule.

Costs and Timing: A Hidden Link
IVF isn’t cheap—$15,000-$20,000 per cycle, says a 2025 Federal Register update. If money’s tight, you might space cycles out, stretching your journey to a year or more. Some states now mandate insurance coverage, so check your options—it could speed things up.
Wrapping It Up: Your IVF Timeline, Your Way
So, how long is the IVF procedure? At its core, one cycle takes 3-6 weeks, but the full ride—from first appointment to baby bump—can be 2 months to a year, depending on your path. It’s a marathon, not a sprint, with twists like your body’s response, tech upgrades, and even your emotional stamina shaping the clock.
The good news? You’re not locked into a rigid schedule. Talk to your doctor, lean on support, and tweak the plan to fit your life. Whether it’s your first shot or a backup cycle, every day brings you closer to your goal. Got questions? Your clinic’s just a call away—and now you’ve got the full scoop to start the conversation.







