How to Avoid Ectopic Pregnancy with IVF: Your Guide to a Safer Journey
Starting a family through in vitro fertilization (IVF) is an exciting step for many, but it comes with its own set of challenges. One concern that often lingers in the back of people’s minds is the risk of an ectopic pregnancy—a situation where the embryo implants outside the uterus, most commonly in the fallopian tubes. While IVF is a powerful tool to help you conceive, it doesn’t completely eliminate this risk. The good news? There are ways to lower your chances and feel more in control of your fertility journey.
In this guide, we’ll walk you through everything you need to know about ectopic pregnancies during IVF, from what causes them to practical steps you can take to avoid them. We’ll dive deeper than most articles out there, offering fresh insights, the latest research, and real-world tips you can actually use. Whether you’re just starting IVF or preparing for your next cycle, this is your go-to resource for staying informed and proactive.
What Is an Ectopic Pregnancy, and Why Does It Happen with IVF?
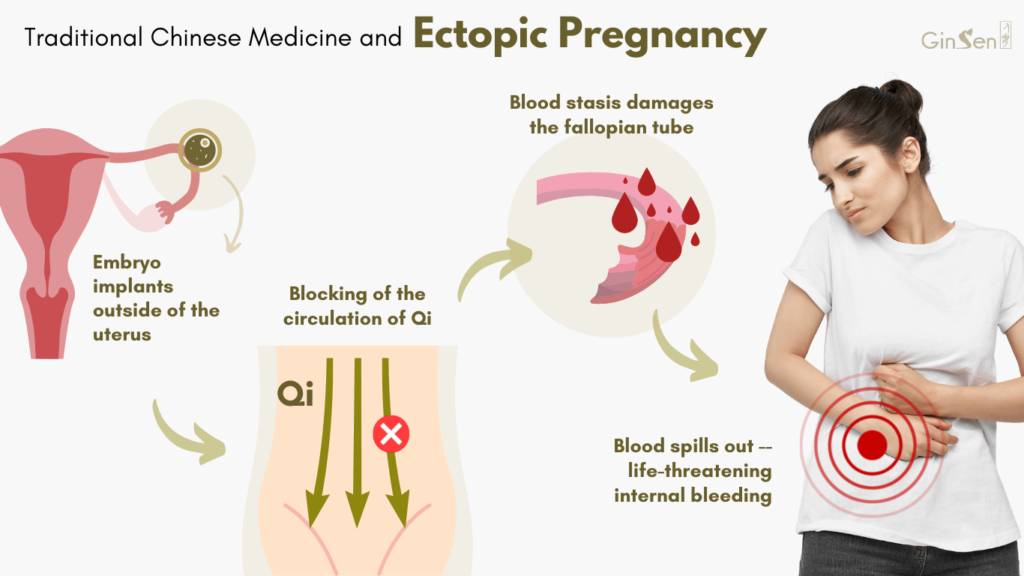
An ectopic pregnancy happens when a fertilized egg settles and grows outside the uterus. Over 90% of the time, this occurs in the fallopian tubes, but it can also happen in the ovaries, cervix, or even the abdominal cavity. Unlike a normal pregnancy, where the embryo implants in the uterine lining, an ectopic pregnancy can’t develop into a healthy baby and can pose serious health risks if not caught early.
You might wonder: if IVF places the embryo directly into the uterus, why does ectopic pregnancy still happen? It’s a fair question! Even with IVF, the embryo can sometimes move out of the uterus after transfer. Think of it like a tiny traveler that doesn’t quite stay where it’s dropped off. Uterine contractions, fluid dynamics, or damaged fallopian tubes can nudge the embryo into the wrong spot. Studies show that ectopic pregnancies occur in about 1-3% of IVF pregnancies—higher than the 1-2% rate in natural conceptions.
The IVF Connection
IVF involves carefully placing embryos into the uterus, bypassing the fallopian tubes entirely. Yet, certain factors—like tubal damage from past infections or surgeries—can increase the odds of an ectopic outcome. Other culprits include transferring multiple embryos or using fresh (not frozen) embryos, which we’ll explore later. The bottom line? While IVF reduces some risks, it doesn’t erase them completely.
Understanding Your Risk Factors: Are You More Prone?
Not everyone faces the same odds of an ectopic pregnancy during IVF. Your personal health history plays a big role. Knowing your risk factors can help you and your doctor make smarter choices to keep things on track.
Common Risk Factors
- Damaged Fallopian Tubes: If you’ve had pelvic inflammatory disease (PID), endometriosis, or tubal surgery, scarring can trap an embryo before it reaches the uterus—or pull it back after transfer.
- Previous Ectopic Pregnancy: If it’s happened before, your risk jumps. Research shows a recurrence rate of about 10-15% in natural pregnancies, and IVF doesn’t fully reset that clock.
- Age: Women over 35 tend to have a slightly higher risk, possibly due to changes in tubal function or hormonal shifts.
- Multiple Embryo Transfers: Transferring more than one embryo can up the chances of one implanting outside the uterus.
IVF-Specific Triggers
Beyond your body’s history, the IVF process itself can influence the outcome. For example, transferring embryos too close to the fallopian tubes (instead of the middle of the uterus) might let them drift. High hormone levels from ovarian stimulation can also mess with uterine contractions, nudging embryos off course.
Quick Quiz: How many of these risk factors apply to you?
- Past tubal issues (e.g., infections, surgeries)
- Over 35 years old
- Planning to transfer multiple embryos
If you checked two or more, it’s worth a chat with your doctor about extra precautions!
How IVF Techniques Impact Ectopic Pregnancy Risk
The way IVF is done can make a difference in whether an ectopic pregnancy happens. Let’s break down the key techniques and what the latest science says about them.
Fresh vs. Frozen Embryo Transfers
Fresh embryo transfers—where embryos are placed in the uterus right after fertilization—used to be the norm. But frozen embryo transfers (FET) are gaining ground, and for good reason. A 2022 study in Fertility and Sterility found that FET cycles have a lower ectopic pregnancy rate (around 1.4%) compared to fresh cycles (up to 2.8%). Why? Frozen transfers give your body time to recover from the intense hormone stimulation of egg retrieval, creating a more natural uterine environment.
✔️ Tip: Ask your clinic about FET if you’re worried about ectopic risks. It might mean a slightly longer wait, but the payoff could be worth it.
Single vs. Multiple Embryo Transfers
Transferring two or more embryos might boost your chances of pregnancy, but it also raises the ectopic risk. A 2023 analysis of over 40,000 IVF cycles showed that double embryo transfers increased ectopic rates by 6 times compared to single transfers in some groups. With single embryo transfer (SET), the risk drops to about 1.6%.
✔️ Tip: Opt for SET if possible, especially if you’re under 38 or have good-quality embryos. It’s safer and still effective.
Embryo Stage: Day 3 vs. Day 5
Embryos can be transferred at the cleavage stage (Day 3) or blastocyst stage (Day 5). Day 5 transfers are stickier—they’re more developed and ready to implant. A 2017 meta-analysis in PLoS One found that Day 5 transfers cut ectopic rates by nearly half compared to Day 3. The catch? Not all embryos make it to Day 5, so your clinic’s lab quality matters.
✔️ Tip: Go for Day 5 transfers if your embryos are strong enough. It’s a small tweak with big benefits.
Practical Steps to Lower Your Risk During IVF
You’re not powerless in this process! Here are actionable steps to minimize your chances of an ectopic pregnancy, based on science and real-world experience.
Step 1: Get Your Tubes Checked
Before starting IVF, ask for a hysterosalpingogram (HSG) or laparoscopy to check your fallopian tubes. If they’re blocked or damaged, your doctor might suggest clipping or removing them (salpingectomy). A 2020 study in European Journal of Obstetrics & Gynecology found that salpingectomy before IVF slashed ectopic rates by 70% in women with tubal issues.
✔️ Action: Schedule a tube check if you’ve had pelvic infections or surgeries. It’s a proactive move that could save you heartache.
Step 2: Optimize Embryo Placement
During the transfer, the doctor uses ultrasound to guide the embryo into the uterus. Studies show placing it 1-2 cm from the top (fundal) edge of the uterus—rather than too deep or near the tubes—lowers ectopic risk. This isn’t something you control directly, but you can ask about it.
✔️ Action: Talk to your doctor about their transfer technique. A skilled hand makes a difference.
Step 3: Balance Your Hormones
High estrogen levels from ovarian stimulation can overstimulate your uterus, increasing contractions that push embryos around. Some clinics now use milder stimulation protocols or “freeze-all” cycles to avoid this.
✔️ Action: Discuss a gentler stimulation plan or freeze-all approach with your team. It’s less stress on your body—and your mind.
Step 4: Monitor Early and Often
Ectopic pregnancies can be caught early with regular check-ins. After your transfer, track your human chorionic gonadotropin (hCG) levels every few days. A slow rise or plateau might signal trouble. An ultrasound at 6 weeks can confirm the embryo’s location.
✔️ Action: Don’t skip follow-ups! Early detection can prevent complications.
Lifestyle Changes That Make a Difference
Your daily habits can support a healthier IVF outcome. These tweaks won’t eliminate ectopic risk entirely, but they can tip the scales in your favor.
Quit Smoking
Smoking damages fallopian tubes and ramps up ectopic risk by 2-3 times, according to the American College of Obstetricians and Gynecologists (ACOG). The chemicals mess with cilia—the tiny hairs that move the embryo along—making it more likely to get stuck.
✔️ Action: Kick the habit before IVF. Even cutting back helps.
Manage Stress
Chronic stress spikes cortisol, which can disrupt hormone balance and uterine function. A 2021 study linked high stress to poorer IVF outcomes, including ectopic pregnancies.
✔️ Action: Try yoga, meditation, or a walk in nature. Small breaks can calm your system.
Watch Your Weight
Being underweight or overweight can throw off your reproductive hormones. A 2023 study of 42,000 IVF cycles found that women with a BMI below 18.5 had a 3.3% ectopic rate—higher than the 2.4% for normal-weight women.
✔️ Action: Aim for a BMI of 18.5-24.9 with a balanced diet and light exercise.
The Emotional Side: Coping with the Fear
Worrying about ectopic pregnancy can cast a shadow over your IVF excitement. It’s normal to feel anxious, but you don’t have to face it alone.
A Real Story
Take Sarah, a 34-year-old who’d had an ectopic pregnancy before IVF. She was terrified it’d happen again. Her doctor suggested a salpingectomy and single frozen embryo transfer. After a smooth cycle, she’s now 20 weeks pregnant with a healthy baby. Sarah’s takeaway? “Knowledge took away half my fear.”
Your Support Plan
- Talk It Out: Share your concerns with your partner, a friend, or a counselor.
- Join a Community: Online forums like Reddit’s r/IVF have folks who get it.
- Focus on What You Can Control: Prep your body, ask questions, and trust your team.
Poll: What’s your biggest IVF worry?
A) Ectopic pregnancy
B) Failed cycle
C) Cost
Drop your answer in your mind—and know you’re not alone!
New Research: What’s Changing the Game?
Science is always evolving, and recent findings offer fresh hope for avoiding ectopic pregnancies in IVF. Here’s what’s new—and how it could help you.
Endometrial Receptivity Testing
This cutting-edge test checks if your uterine lining is ready for implantation. A 2024 pilot study found that timing transfers to your “receptive window” cut ectopic rates by 30%. It’s not standard yet, but it’s worth asking about.
✔️ Insight: If your lining’s off, embryos might not stick where they should. This could be a game-changer.
AI-Powered Embryo Selection
Artificial intelligence is helping doctors pick the healthiest embryos. A 2023 trial showed AI-selected embryos had a 25% lower ectopic rate than traditional methods. Why? Better embryos implant more reliably.
✔️ Insight: Ask if your clinic uses AI tools—it’s not sci-fi anymore!
Tubal Flushing with Oil
An old technique is making a comeback. Flushing fallopian tubes with an oil-based contrast before IVF can clear debris and reduce ectopic risk by up to 40%, per a 2022 Dutch study.
✔️ Insight: It’s low-tech but effective. Could it work for you?
Busting Myths: What Doesn’t Cause Ectopic Pregnancy
There’s a lot of noise out there about ectopic pregnancies. Let’s clear up some misconceptions so you can focus on what matters.
❌ Myth: IVF always causes ectopic pregnancies.
Truth: The risk is higher than natural conception, but it’s still low (1-3%). Most IVF pregnancies implant just fine.
❌ Myth: Stress alone triggers ectopic pregnancies.
Truth: Stress can affect outcomes, but it’s not a direct cause. It’s more about physical factors like tubal health.
❌ Myth: You can’t prevent it—it’s just bad luck.
Truth: While luck plays a role, smart choices (like SET or FET) can lower your odds.
Your IVF Action Plan: A Step-by-Step Guide
Ready to take charge? Here’s a clear roadmap to minimize ectopic risk, from prep to post-transfer.
Before IVF
- Screen Your Tubes: Get an HSG or laparoscopy to spot issues.
- Fix What You Can: Consider salpingectomy if tubes are damaged.
- Lifestyle Tune-Up: Quit smoking, eat well, and de-stress.
During IVF
- Choose Wisely: Go for single, frozen, Day 5 transfers if possible.
- Ask Questions: Confirm the embryo placement technique with your doctor.
- Stay Calm: Use relaxation techniques during the two-week wait.
After Transfer
- Track hCG: Watch for slow rises—call your clinic if something’s off.
- Early Ultrasound: Schedule one at 6 weeks to check placement.
- Rest Easy: Follow your doctor’s advice, but don’t overdo bed rest—it doesn’t help implantation.
A Deeper Dive: Why Tubal Health Matters More Than You Think
Most articles skim over tubal health, but it’s a hidden key to avoiding ectopic pregnancies. Damaged tubes don’t just block the embryo’s path—they can actively pull it back after transfer. How? Pressure differences between the uterus and tubes create a suction effect, especially if there’s scarring or fluid buildup (hydrosalpinx).
A 2021 study in Human Reproduction found that women with hydrosalpinx had a 5% ectopic rate—triple the average—unless it was treated first. Clipping or removing the affected tube dropped that risk to near zero. This isn’t talked about enough, but it’s a critical piece of the puzzle.
✔️ Takeaway: If your tubes are suspect, don’t skip the fix. It’s not just about getting pregnant—it’s about staying safe.
The Future of IVF: What’s on the Horizon?
IVF is getting smarter, and that means fewer ectopic pregnancies down the road. Beyond AI and endometrial testing, researchers are exploring uterine “mapping” with 3D ultrasound to pinpoint the perfect transfer spot. Early trials suggest it could cut ectopic rates by 20%. Meanwhile, gene editing might one day fix tubal damage at the cellular level—though that’s years away.
For now, the focus is on precision: better tools, better timing, better outcomes. You’re part of a generation that’s pushing fertility science forward.
Wrapping Up: Your Path to a Safer IVF Pregnancy
Ectopic pregnancy is a real concern with IVF, but it’s not the whole story. By understanding your risks, tweaking the process, and staying proactive, you can tilt the odds in your favor. This isn’t about fear—it’s about empowerment. You’ve got the tools, the science, and a team behind you to make this work.
So, take a deep breath. Talk to your doctor about single frozen transfers, tubal health, and early monitoring. Make those lifestyle tweaks. And most importantly, hold onto hope. Your journey might have twists, but with the right steps, it can lead to the family you’ve been dreaming of.
Checklist: What’s your next move?
- Schedule a tubal check
- Ask about frozen transfers
- Start a stress-busting routine
Pick one and go for it—you’ve got this!







