What Are IVF Treatments? Your Complete Guide to Understanding In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about starting a family, especially when things don’t go as planned. It’s a process that’s helped millions of people worldwide become parents, and it’s more common than you might think—about 1-2% of all babies born in the U.S. each year come from IVF. But what exactly is it? How does it work, and why do people turn to it? If you’re curious about IVF treatments or wondering if they might be an option for you, you’re in the right place. This guide will walk you through everything you need to know, from the basics to the nitty-gritty details, with a few surprises along the way.
IVF isn’t just a medical procedure—it’s a journey. It’s a mix of science, hope, and a little bit of patience. Whether you’re dealing with infertility, exploring family-building options as a single person or same-sex couple, or just want to know more, this article will break it all down in a way that’s easy to follow. We’ll cover how IVF works step-by-step, who it’s for, what it feels like (emotionally and physically), and even some lesser-known facts that don’t always make it into the headlines. Plus, we’ll sprinkle in some practical tips and the latest insights to give you a fuller picture than you’ll find anywhere else.
So, grab a comfy seat, maybe a cup of tea, and let’s dive into the world of IVF treatments together.
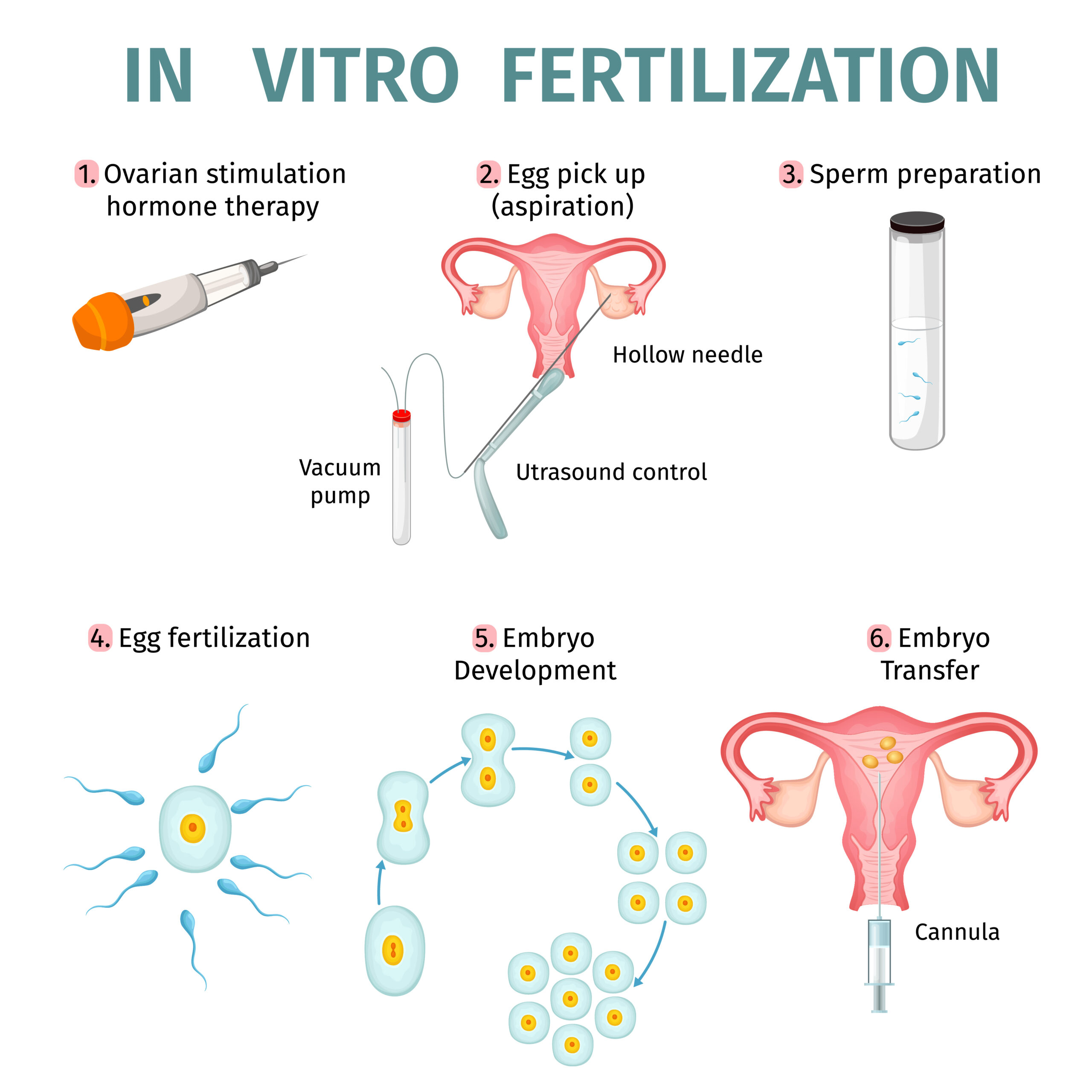
How IVF Treatments Work: A Step-by-Step Breakdown
IVF stands for “in vitro fertilization,” which is a fancy way of saying “fertilization in a glass.” The “glass” part refers to a lab dish where eggs and sperm meet, not inside the body like in natural conception. It’s a multi-step process that can take a few weeks to a couple of months, depending on your situation. Here’s how it unfolds:
Step 1: Boosting Egg Production
The journey starts with your ovaries. Normally, your body releases one egg a month during ovulation. With IVF, doctors want more eggs to increase the chances of success. You’ll take hormone injections—usually for about 8-14 days—to stimulate your ovaries to produce multiple eggs at once. These shots might sound intimidating, but they’re just tiny needles you can often do at home. Your doctor will monitor you with ultrasounds and blood tests to see how those eggs are growing.
Step 2: Collecting the Eggs
Once your eggs are ready (think of them as little ripened fruits), it’s time for retrieval. This is a quick procedure—about 20-40 minutes—done under light anesthesia. A doctor uses an ultrasound-guided needle to gently pull the eggs from your ovaries through your vaginal wall. It’s not as scary as it sounds; most people say it’s like a deep nap with some mild cramping afterward. On average, 10-15 eggs are collected, though this varies.
Step 3: Fertilizing the Eggs
Now comes the magic moment. In a lab, your eggs meet the sperm—either from your partner or a donor. There are two ways this can happen:
- Traditional IVF: The eggs and sperm are mixed in a dish, and nature takes its course.
- ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected directly into an egg, often used if sperm quality is low.
After fertilization, the eggs become embryos and grow in the lab for 3-5 days. Scientists keep a close eye on them to pick the healthiest ones.
Step 4: Transferring the Embryo
A few days later, one or two embryos are placed into your uterus using a thin tube called a catheter. It’s a simple, painless process—no anesthesia needed—and feels a bit like a Pap smear. If an embryo implants in your uterine lining, you’re pregnant! About 10-14 days later, a blood test confirms it.
Step 5: The Waiting Game
This part’s tough: the “two-week wait.” You’ll wonder about every twinge or symptom. Some embryos might be frozen for later use if you have extras, which is handy for future tries or siblings down the road.
That’s the basic roadmap. Each step is tailored to you—your age, health, and fertility challenges—so it’s not one-size-fits-all. Pretty cool how science steps in to give nature a nudge, right?
Who Needs IVF? More People Than You Might Think
IVF isn’t just for one type of person. It’s a tool that helps all kinds of people build families when the usual way doesn’t work. Here’s who might turn to IVF:
Couples Facing Infertility
About 1 in 8 couples struggle to conceive naturally. IVF can help with issues like:
- Blocked fallopian tubes: If the tubes are damaged (say, from an infection), eggs can’t reach the uterus. IVF bypasses this.
- Low sperm count or motility: If sperm can’t swim well or there aren’t enough, IVF (especially with ICSI) can make fertilization happen.
- Endometriosis: This condition can mess with egg quality or implantation, and IVF often improves the odds.
- Unexplained infertility: Sometimes, there’s no clear reason, but IVF can still work.
Single Parents and Same-Sex Couples
You don’t need a partner to have a baby with IVF. Single women can use donor sperm, while same-sex female couples might use one partner’s eggs and a donor’s sperm. For male couples, IVF pairs with surrogacy—using donor eggs and a gestational carrier.
People Preserving Fertility
If you’re facing cancer treatment or want to delay parenthood, IVF lets you freeze eggs or embryos. Women in their 30s or 40s often freeze eggs to beat the biological clock, since fertility drops after 35. In 2021, the CDC reported over 20,000 egg-freezing cycles in the U.S. alone.
Those Avoiding Genetic Disorders
IVF can screen embryos for conditions like cystic fibrosis or Down syndrome before transfer, using a process called preimplantation genetic testing (PGT). It’s a game-changer for families with a history of genetic issues.
No matter the reason, IVF opens doors that might otherwise stay closed. It’s not just about infertility—it’s about possibilities.
What Does IVF Feel Like? The Emotional and Physical Ride
IVF isn’t just a physical process; it’s an emotional rollercoaster too. Knowing what to expect can make it less overwhelming.
The Physical Side
- Hormone Shots: You might feel bloated, moody, or tired from the meds. Some get mild headaches or sore spots from injections.
- Egg Retrieval: Post-procedure, expect cramping (like period pain) and maybe some spotting. It fades in a day or two.
- Embryo Transfer: Super easy—no pain, just a quick visit.
- Side Effects: Rarely, ovarian hyperstimulation syndrome (OHSS) can happen, causing swelling or discomfort. It affects less than 5% of cases and is treatable.
The Emotional Side
- Hope and Anxiety: You’re excited but nervous. Every step feels like a milestone—and a cliffhanger.
- The Two-Week Wait: This is the hardest part. You might overanalyze every symptom, swinging between optimism and doubt.
- Support Matters: Studies show emotional support boosts success rates. One 2020 study found couples with strong social networks had a 15% higher chance of conceiving via IVF.
Quick Tip: Keep a journal or talk to a friend. It helps process the ups and downs.
How Successful Is IVF? Numbers That Tell the Story
Success rates depend on a lot—your age, health, and even the clinic. Here’s what the latest data says (from the CDC’s 2021 ART Report):
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 44.5% |
| 35-37 | 32.4% |
| 38-40 | 20.1% |
| 41-42 | 9.7% |
| Over 42 | 2.9% |
- Younger is Better: Under 35, you’ve got nearly a 50-50 shot per cycle. After 40, it drops fast due to egg quality.
- Frozen Embryos: Using frozen embryos from a prior cycle can hit 40% success across ages, thanks to better freezing tech.
- Multiple Cycles: Most people need 2-3 cycles. Cumulative success after three tries can reach 60-70% for younger patients.
Fun Fact: In 2023, a new AI tool called Life Whisperer improved embryo selection, boosting success by up to 10% in some clinics. Tech is changing the game!

The Cost of IVF: What You’re Really Paying For
IVF isn’t cheap, but understanding the breakdown helps. In the U.S., one cycle averages $15,000-$20,000. Here’s where the money goes:
- Meds: $3,000-$5,000 for hormone shots.
- Monitoring: $1,000-$2,000 for ultrasounds and blood tests.
- Egg Retrieval: $5,000-$7,000, including anesthesia.
- Lab Work: $3,000-$5,000 to fertilize and grow embryos.
- Transfer: $1,000-$2,000 for the final step.
Hidden Costs
- Extra Cycles: Many need more than one try.
- Freezing: Storing embryos costs $500-$1,000 a year.
- Travel: If your clinic’s far, add gas or flights.
Making It Affordable
- Insurance: Only 19 states mandate some IVF coverage. Check your plan!
- Grants: Groups like Baby Quest offer up to $15,000.
- Mini IVF: A lower-dose option can cut costs to $5,000-$7,000, though success rates may dip.
Money’s a big hurdle, but options exist. It’s worth shopping around—clinics vary widely in price and payment plans.
IVF Myths vs. Facts: Clearing the Air
There’s a lot of noise about IVF. Let’s sort truth from fiction:
Myth 1: IVF Babies Have More Birth Defects
Fact: Early studies hinted at a slight risk, but 2022 research from the American Society for Reproductive Medicine shows IVF babies are just as healthy as naturally conceived ones. The key? Screening embryos with PGT reduces risks.
Myth 2: IVF Always Means Twins
Fact: Not anymore. Clinics now push single embryo transfers to avoid multiples. Twins happen in less than 15% of IVF births today, down from 30% a decade ago.
Myth 3: It’s Only for Older Women
Fact: Nope! People in their 20s use IVF for genetic screening or medical issues. Age doesn’t define the need.
Quick Quiz: Think IVF is just for couples? Who else uses it? (Answer: Single folks, same-sex couples, and fertility preservers!)
Three Things You Didn’t Know About IVF (But Should)
Most articles skim the surface. Here are three under-the-radar insights that add depth:
1. Your Diet Can Boost IVF Success
A 2023 study from Harvard found women eating a Mediterranean diet—think olive oil, fish, and veggies—had a 20% higher success rate. Why? It reduces inflammation and supports egg quality. Swap out processed snacks for nuts and see the difference.
2. Men’s Health Matters Too
Sperm quality isn’t just about count. A 2024 Australian study linked high oxidative stress in men (from smoking or poor diet) to lower IVF success. Guys, ditch the junk food and add antioxidants like vitamin C—your embryos will thank you.
3. Timing Isn’t Everything
Old wisdom said embryos had to implant in a narrow “window.” New research from 2024 suggests embryos might adapt to the uterus better than we thought, even days off-schedule. This could mean more flexible transfer dates soon.
These nuggets show IVF’s more than just shots and lab dishes—it’s a team effort between you, your body, and science.
IVF Around the World: A Global Snapshot
IVF isn’t the same everywhere. Here’s how it varies:
- U.S.: High-tech but pricey. No national coverage, so it’s a patchwork of insurance and out-of-pocket costs.
- UK: The NHS offers up to three free cycles if you’re under 40 and meet criteria. Private cycles run $6,000-$8,000.
- India: A hotspot for affordable IVF—$2,000-$3,000 per cycle. It’s why “fertility tourism” is booming there.
- Israel: Tops the world with 1,600+ cycles per million people yearly. Subsidies cover up to two kids.
Did You Know? In Japan, a 2023 policy shift now funds six cycles for women under 43, reflecting a push to boost birth rates.
The Emotional Toolkit: Coping with IVF
IVF can feel like a marathon. Here’s how to stay strong:
Build Your Squad
- ✔️ Lean on friends who get it—maybe someone who’s been through IVF.
- ✔️ Join an online group. Instagram’s #IVFcommunity has over 500,000 posts of real stories.
- ❌ Don’t isolate. Silence breeds stress.
Manage the Wait
- ✔️ Try mindfulness—5 minutes of deep breathing daily cuts anxiety, per a 2021 study.
- ❌ Avoid symptom Googling. It’s a rabbit hole of false hope.
Celebrate Small Wins
- ✔️ Got through retrieval? Treat yourself to ice cream.
- ✔️ Embryos made it to day 5? High-five your partner.
Poll: What’s your go-to stress buster? Share in the comments—yoga, Netflix, or a good cry?

The Future of IVF: What’s Next?
IVF’s evolving fast. Here’s what’s on the horizon:
AI-Powered Embryo Selection
Tools like Life Whisperer use AI to pick the best embryos, cutting guesswork. Early adopters report a 10-15% success bump.
Lab-Grown Eggs
Scientists are testing ways to make eggs from stem cells. A 2024 breakthrough in mice hints this could help women with no viable eggs in a decade.
At-Home Monitoring
Imagine tracking your cycle with a smartphone app and a tiny sensor. Prototypes are in trials—less clinic time, more comfort.
These advances could make IVF cheaper, faster, and more accessible. The future’s looking bright!
Real Stories: IVF in Action
Meet Sarah, a 34-year-old teacher from Ohio. After two years of trying naturally, she and her husband found out his sperm motility was low. IVF with ICSI gave them a healthy boy in 2023. “The shots were rough, but seeing that heartbeat made it worth it,” she says.
Then there’s James, a single dad in California. At 38, he used donor eggs and a surrogate via IVF. “I never thought I’d be a parent alone, but IVF made it real,” he shares. His daughter’s now 2.
These stories remind us: IVF’s not just science—it’s people chasing dreams.
Your IVF Action Plan: Where to Start
Ready to explore IVF? Here’s a simple roadmap:
- Talk to Your Doctor: Get a fertility check—blood tests and a semen analysis reveal a lot.
- Find a Clinic: Look for high success rates and good reviews. The CDC’s ART tool lists stats by clinic.
- Ask About Costs: Get a full quote, including meds and extras.
- Prep Your Body: Eat well, sleep more, and cut stress—small changes add up.
- Build Support: Tell a friend or join a group. You’re not alone.
Checklist:
- ✔️ Booked a consult?
- ✔️ Researched clinics?
- ✔️ Got a savings plan?
Start small, but start now. Every step brings you closer.







