What Does IVF Mean for You? A Deep Dive into In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about starting a family, especially if getting pregnant the usual way isn’t working out. But what does IVF really mean—not just in a textbook definition, but for real people like you who might be thinking about it? It’s more than just science in a lab; it’s a journey, a hope, and sometimes a rollercoaster of emotions. Whether you’re curious, researching options, or ready to take the plunge, this article is here to walk you through what IVF is, how it works, and what it could mean for your life—without the jargon overload.
IVF has been around since the late 1970s, when the first “test-tube baby,” Louise Brown, was born in England. Since then, it’s helped millions of people become parents—over 8 million babies worldwide, according to recent estimates. But it’s not a one-size-fits-all solution, and it’s definitely not a quick fix. Let’s break it down step by step, explore the latest trends, and dig into some angles you won’t find in every article out there.
What Is IVF, Exactly?
IVF stands for in vitro fertilization, which is Latin for “in glass.” That’s because it happens outside the body, in a lab dish, where an egg and sperm meet up under a microscope. Think of it like giving nature a little nudge when it’s not happening on its own. It’s one of the most well-known types of assisted reproductive technology (ART), a fancy term for medical tricks that help people conceive.
Here’s the basic gist: doctors take eggs from a woman’s ovaries, mix them with sperm in a lab, and then place the resulting embryo (a fertilized egg) back into the uterus to grow into a baby. It sounds simple, but there’s a lot going on behind the scenes—hormone shots, precise timing, and some pretty cool science.
Why People Turn to IVF
People choose IVF for all kinds of reasons. Maybe the fallopian tubes are blocked, so the egg and sperm can’t meet naturally. Or perhaps sperm count is low, making it tough for fertilization to happen. Sometimes, it’s just a mystery—unexplained infertility—where everything seems fine but pregnancy isn’t clicking. Other times, it’s about timing, like women freezing their eggs to have kids later or couples using a surrogate.
IVF isn’t just for straight couples, either. Single folks and same-sex couples use it too, often with donor eggs, sperm, or embryos. It’s a tool that’s opened doors for all kinds of families, which is pretty amazing when you think about it.
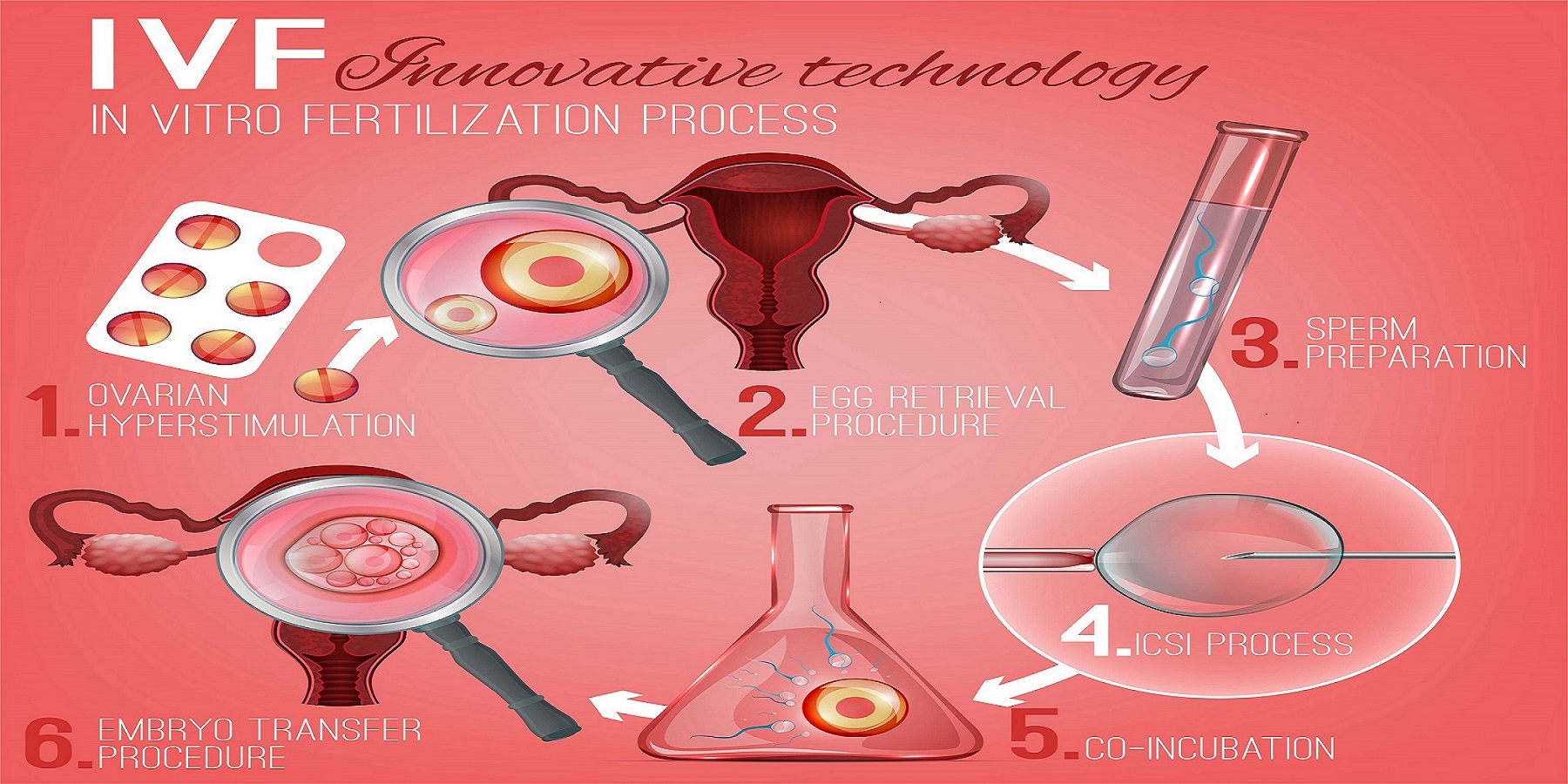
How Does IVF Work? A Step-by-Step Look
IVF isn’t a one-day deal—it’s a process that takes weeks and involves a team of doctors, nurses, and lab experts. Here’s what happens, broken down into bite-sized pieces so you can picture it.
Step 1: Boosting Egg Production
Normally, your ovaries release one egg a month. With IVF, doctors want more eggs to work with, so they use hormone injections to kick your ovaries into overdrive. These shots—like follicle-stimulating hormone (FSH)—tell your body to grow multiple eggs at once. You’ll get these for about 10-14 days, and yes, they can make you feel bloated or moody. Doctors keep an eye on things with ultrasounds and blood tests to see how those eggs are coming along.
✔️ Tip: Keep a journal during this phase—tracking how you feel can help you manage the ups and downs.
Step 2: Collecting the Eggs
Once the eggs are ready, it’s time to get them out. This is called egg retrieval, and it’s a minor procedure done under light sedation. A doctor uses a thin needle, guided by ultrasound, to pull the eggs from your ovaries through your vagina. It takes about 20-30 minutes, and you’ll rest afterward. On average, they might collect 10-15 eggs, though it varies.
❌ Heads-up: You might feel crampy or spot a little blood after—totally normal, but call your doctor if it’s intense.
Step 3: Fertilizing the Eggs
Now the lab magic happens. The eggs meet the sperm—either from a partner or a donor—in a dish. There are two ways this can go:
- Traditional IVF: Sperm and eggs are mixed together and left to do their thing.
- ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected right into an egg, used when sperm quality is low.
After a day or two, the team checks to see if fertilization worked. If it did, you’ve got embryos!
Step 4: Growing the Embryos
The embryos chill in the lab for 3-5 days, growing from a few cells to a blastocyst (a more developed stage). Doctors watch them closely, picking the healthiest ones for transfer. Extra embryos can be frozen for later—think of it like a backup plan.
Step 5: Transferring the Embryo
This part’s quick and painless. A doctor slides a thin tube through your cervix and places one or two embryos into your uterus. No anesthesia needed—you’re awake and might even watch on an ultrasound screen. Then, you wait about two weeks to take a pregnancy test.
✔️ Pro move: Rest after the transfer, but don’t stress about lying flat all day—studies show normal activity is fine.
What’s New in IVF? Trends and Tech You Should Know
IVF isn’t stuck in the 1970s—it’s evolving fast. Here’s what’s hot in 2025, based on the latest buzz and research.
Less Invasive Options
Some clinics now offer “mild IVF” or “natural cycle IVF,” using fewer drugs or none at all. It’s gentler on your body and cheaper, though success rates can be lower—around 10-15% per cycle versus 25-30% with standard IVF, per the American Society for Reproductive Medicine (ASRM). It’s a trade-off worth considering if you’re wary of hormones.
Embryo Screening Gets Smarter
Preimplantation genetic testing (PGT) lets doctors check embryos for genetic issues before transfer. Newer tech, like AI-powered imaging, is making this faster and more accurate. A 2024 study from Nature found AI can predict embryo viability with 85% accuracy, up from 70% with human judgment alone.
Freezing for the Future
Egg freezing is booming, especially for women in their 30s who want kids later. Clinics are perfecting vitrification—a flash-freezing method that keeps eggs in top shape. Over 50,000 women froze their eggs in the U.S. in 2023, double the number from five years ago, says the Society for Assisted Reproductive Technology (SART).
What Are the Odds? Success Rates and Real Talk
IVF success isn’t a guarantee, and the numbers depend on a lot—your age, health, and even luck. Here’s a snapshot based on 2023 SART data:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 45-50% |
| 35-37 | 35-40% |
| 38-40 | 25-30% |
| Over 40 | 10-15% |
For context, natural conception has a 20-25% chance per month for women under 30, dropping as you age. IVF beats that for younger folks, but it’s not a slam dunk.
What Boosts Your Chances?
- Healthy lifestyle: Quit smoking, cut back on booze, and keep your weight in check—studies link these to better outcomes.
- Fresh vs. frozen: Fresh embryo transfers edge out frozen ones slightly (48% vs. 43% for under-35s), but frozen is catching up.
- Clinic quality: Pick a place with a solid track record—check their SART stats online.
❌ Don’t fall for this: Some clinics hype “miracle” add-ons like embryo glue or time-lapse imaging. Research from the Human Fertilisation and Embryo Authority (HFEA) in 2024 says most lack strong evidence of boosting success.
The Emotional Side: What IVF Feels Like
IVF isn’t just physical—it’s a mental marathon. You might feel hopeful one day, crushed the next. A 2023 study in Fertility and Sterility found 60% of IVF patients report anxiety or depression during treatment. That’s why support matters.
Coping Tips from Real People
- Talk it out: Join a support group—online ones on X are buzzing with folks sharing stories.
- Set boundaries: Tell family when you need space; not everyone gets it.
- Celebrate small wins: Got through egg retrieval? Treat yourself to ice cream.
Quick Quiz: How do you unwind?
A) Netflix binge
B) Long walk
C) Call a friend
D) Other (tell us in your head!)
Whatever works, lean into it—IVF’s a lot, and you deserve a break.
Costs and Coverage: What’s the Damage?
IVF isn’t cheap. In the U.S., one cycle averages $15,000-$20,000, including meds. Insurance varies wildly—19 states mandate some coverage, but loopholes abound. Globally, costs drop in places like Spain ($5,000-$7,000) or India ($3,000-$5,000), fueling “fertility tourism.”
Money-Saving Hacks
- Mini-IVF: Less meds, lower cost—around $7,000-$10,000.
- Grants: Groups like Baby Quest offer up to $15,000 for eligible applicants.
- Shared risk programs: Some clinics refund part of the fee if it fails after multiple tries.
✔️ Try this: Map out a budget before you start—factor in meds, travel, and time off work.
Risks and Realities: What Could Go Wrong?
IVF is safe overall, but it’s not risk-free. Here’s what to watch for, backed by science.
Physical Risks
- Ovarian Hyperstimulation Syndrome (OHSS): Too many eggs can swell your ovaries—happens in 1-5% of cycles, per the Mayo Clinic. Mild cases mean bloating; severe ones need a doctor ASAP.
- Multiple births: Twins or triplets sound cute, but they raise preterm birth risks—about 20% of IVF pregnancies are multiples.
- Ectopic pregnancy: The embryo implants outside the uterus in 2-5% of cases—rare but serious.
Long-Term Questions
Does IVF affect your health years later? A 2024 study in The Lancet tracked 10,000 IVF moms over 20 years and found no higher cancer risk tied to the hormones. Kids born via IVF? They’re just as healthy as their peers, per a 2023 Pediatrics review of 50,000 cases.
IVF Myths Busted: What’s True, What’s Not
There’s a lot of noise out there. Let’s clear it up.
- Myth: IVF babies are “unnatural.”
Truth: They’re conceived differently, but they’re 100% human—same DNA, same potential. - Myth: IVF always works on the first try.
Truth: Most people need 2-3 cycles—patience is key. - Myth: It’s only for older women.
Truth: Plenty of 20- and 30-somethings use it for medical or personal reasons.
Three Things You Haven’t Heard About IVF
Most articles stick to the basics, but here’s some fresh ground to cover.
1. The Microbiome Connection
Your gut might play a role in IVF success. A 2024 study in Reproductive Sciences found women with balanced gut bacteria had a 10% higher implantation rate. Probiotics aren’t a cure-all, but eating yogurt or fermented foods could be a low-key boost.
✔️ Action step: Add a daily serving of kefir or kimchi—can’t hurt, might help.
2. Sperm’s Hidden Struggles
We talk eggs a lot, but sperm quality’s half the equation. New research shows heat stress—like from laptops or hot tubs—can tank sperm DNA integrity, cutting IVF success by up to 15% (Journal of Andrology, 2025). Guys, keep it cool down there.
❌ Avoid this: Skip the sauna during treatment—give those swimmers a break.
3. The “Quiet Embryo” Theory
Not all embryos make noise—metaphorically. A 2024 paper from Stanford suggests some top-quality embryos don’t grow fast or look flashy under a microscope but still lead to healthy babies. Clinics might overlook them, so ask about “slow growers” if you’re digging into options.
Your IVF Game Plan: Practical Steps to Start
Ready to explore IVF? Here’s how to kick things off without feeling lost.
Step 1: Find a Clinic
Look up SART or HFEA ratings online—pick a place with good stats and reviews. Call for a consult; most offer a free first chat.
Step 2: Ask the Right Questions
- What’s your success rate for my age?
- Do you offer mild IVF or financing?
- How do you handle emotional support?
Step 3: Prep Your Body and Mind
- Eat well: Think Mediterranean—fish, veggies, nuts.
- Sleep: Aim for 7-8 hours; it regulates hormones.
- De-stress: Yoga or meditation can lower cortisol, which messes with fertility.
Poll Time: What’s your biggest IVF worry?
A) Cost
B) Success odds
C) Side effects
D) Something else
Jot it down mentally—we’re all in this together.
Real Stories: IVF in Action
Numbers are great, but stories hit home. Meet Sarah and Mike (names changed), a couple from Ohio. After two years of trying, they turned to IVF at 32. First cycle failed—tough blow. Second try, with a frozen embryo, worked. Their son’s 3 now, and they’re planning for number two. “It’s not easy,” Sarah says, “but seeing him smile makes every shot worth it.”
Then there’s Priya, a single 38-year-old in California. She froze her eggs at 34, used a sperm donor, and had twins via IVF last year. “I didn’t wait for a partner,” she says. “IVF let me build my family my way.”
The Future of IVF: What’s Next?
IVF’s not done evolving. Labs are testing “lab-on-a-chip” tech to automate embryo growth, cutting costs and human error. Gene editing (like CRISPR) is on the horizon, though it’s controversial—could it prevent diseases before birth? And socially, IVF’s stigma is fading fast—X posts in 2025 show more people openly sharing their journeys.







