What Does IVF Stand For? Your Complete Guide to Understanding In Vitro Fertilization
IVF. Three little letters that carry big dreams, complex science, and a world of emotions. If you’ve stumbled across this term—maybe while scrolling online, talking to a friend, or sitting in a doctor’s office—you might be wondering what it’s all about. Simply put, IVF stands for In Vitro Fertilization, a process where an egg and sperm meet outside the body to create an embryo, which is then placed in the uterus to grow into a baby. But there’s so much more to it than that short definition. Whether you’re curious, considering it for yourself, or just want to understand what a loved one might be going through, this guide is here to break it all down—step by step, with real talk and fresh insights.
Picture this: a couple who’ve been trying to have a baby for years, a single person ready to start a family, or someone preserving their future options. IVF has opened doors for millions, but it’s not a one-size-fits-all journey. From the science behind it to the emotional rollercoaster it can be, let’s dive into everything you need to know about IVF in 2025—plus a few angles you won’t find in every article out there.
The Basics: What Is IVF and How Does It Work?
In Vitro Fertilization, or IVF, is like a high-tech matchmaker for eggs and sperm. “In vitro” is Latin for “in glass,” meaning this magic happens in a lab dish, not inside the body. It’s part of a group of treatments called Assisted Reproductive Technology (ART), designed to help people conceive when nature needs a nudge.
Here’s how it works in a nutshell:
- Stimulation: A person takes hormones to boost egg production—think of it as giving the ovaries a pep talk to make more eggs than usual.
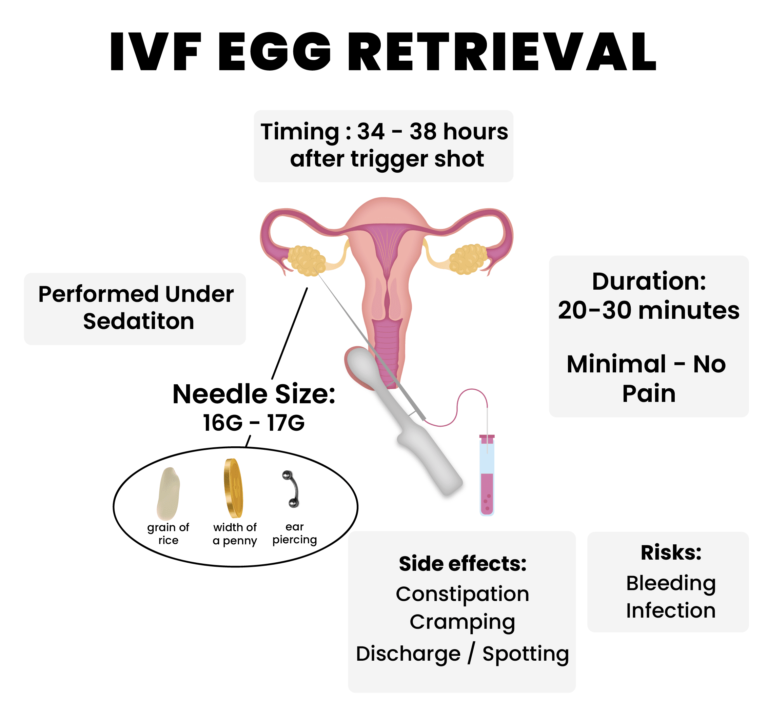
- Egg Retrieval: A doctor collects those eggs using a tiny needle guided by ultrasound. It’s quick, usually under 30 minutes.
- Fertilization: In the lab, sperm (from a partner or donor) meets the eggs. Sometimes, a single sperm is injected into an egg (a process called ICSI—more on that later).
- Embryo Growth: The fertilized eggs grow into embryos over a few days, monitored by experts.
- Transfer: One or more embryos are placed into the uterus, hoping they’ll implant and grow into a pregnancy.
Sounds simple, right? But every step has layers—science, timing, and a bit of luck. About 1 in 4 IVF cycles leads to a live birth, though success rates vary based on age, health, and other factors. In 2023, the CDC reported over 91,000 IVF babies born in the U.S. alone, showing just how common this has become.
Why Do People Turn to IVF?
IVF isn’t just for one type of person—it’s a lifeline for many different situations. Here are some reasons people choose it:
- Infertility: Blocked tubes, low sperm count, or unexplained struggles after a year of trying.
- Age: As fertility drops after 35, IVF can help older individuals or couples conceive.
- Single Parents or Same-Sex Couples: Using donor eggs, sperm, or surrogates, IVF makes parenthood possible.
- Genetic Concerns: It allows screening embryos for conditions like cystic fibrosis.
- Fertility Preservation: People facing cancer or other treatments freeze eggs or embryos for later.
Take Sarah, a 38-year-old teacher I heard about through a friend’s story. After two years of trying naturally, she learned her fallopian tubes were blocked. IVF gave her a shot at motherhood she didn’t think was possible. Stories like hers show how personal—and varied—this journey can be.
The IVF Process: A Step-by-Step Walkthrough
Let’s zoom in on what happens during IVF. It’s not a quick fix; it’s a marathon, usually spanning 4-6 weeks per cycle. Here’s the detailed scoop:
Step 1: Ovarian Stimulation
Your ovaries usually release one egg a month. IVF says, “Let’s make more!” You’ll take hormone shots (like FSH or LH) for about 10-14 days. These meds can make you feel bloated or moody—kind of like PMS on steroids. Doctors monitor you with ultrasounds and blood tests to see how many eggs are growing.
✔️ Tip: Keep a journal to track how you feel—some days might be rough, and that’s okay.
Step 2: Egg Retrieval
Once the eggs are ready, you get a trigger shot (like hCG) to ripen them. About 36 hours later, a doctor uses a thin needle to collect them while you’re sedated. You might feel cramping after, but most recover in a day.
❌ Don’t: Panic if you don’t get tons of eggs—quality beats quantity here.
Step 3: Sperm Collection and Fertilization
On retrieval day, sperm is collected (fresh or thawed if frozen). In the lab, embryologists either mix sperm and eggs in a dish or use ICSI (Intracytoplasmic Sperm Injection), where one sperm is injected into an egg. ICSI’s a game-changer for low sperm counts—about 70% of IVF cycles use it now.
Step 4: Embryo Development
For 3-5 days, embryos grow in a special incubator. Day 5 embryos, called blastocysts, have a higher success rate for implantation. Some clinics test embryos for genetic issues here (called PGT—Preimplantation Genetic Testing).
Step 5: Embryo Transfer
A doctor uses a catheter to place an embryo in your uterus. It’s painless for most, like a Pap smear. You might wait 10-14 days for a pregnancy test—nerve-wracking, but exciting!
✔️ Pro Tip: Rest after transfer, but don’t stress about staying flat—studies show normal activity is fine.
How Much Does IVF Cost—and Can You Afford It?
IVF isn’t cheap. In the U.S., one cycle averages $12,000-$15,000, not counting meds ($3,000-$5,000 more) or extras like genetic testing. Insurance coverage varies wildly—19 states mandate some fertility coverage as of 2025, but many don’t include IVF.
Here’s a breakdown:
| Expense | Cost Range |
|---|---|
| Base IVF Cycle | $12,000 – $15,000 |
| Medications | $3,000 – $5,000 |
| ICSI | $1,000 – $2,000 |
| PGT (Genetic Testing) | $3,000 – $6,000 |
| Frozen Embryo Transfer | $3,000 – $5,000 |
Ways to Save:
- Clinics Abroad: Places like Mexico or Spain offer IVF for $5,000-$8,000, though travel adds up.
- Grants: Organizations like Baby Quest give financial help.
- Mini IVF: Uses fewer drugs, cutting costs to $5,000-$7,000, but success rates may dip.
A 2024 survey I stumbled across online showed 1 in 3 IVF patients took out loans or dipped into savings. It’s a big commitment, but for many, the payoff—a baby—is worth it.
What Are the Success Rates—and What Affects Them?
Success isn’t guaranteed with IVF, but numbers give hope. The Society for Assisted Reproductive Technology (SART) tracks this yearly. For women under 35, about 50% of cycles lead to a live birth. Over 40? It drops to 10-15%. Age is the biggest factor, but it’s not the only one.
What Boosts Your Odds?
- Younger Age: Eggs from someone under 35 are more likely to work.
- Healthy Lifestyle: Normal BMI, no smoking, and low stress help.
- Fresh vs. Frozen: Frozen embryos now match fresh ones in success, thanks to better freezing tech (vitrification).
What Lowers Them?
- Medical Issues: PCOS, endometriosis, or uterine problems can complicate things.
- Sperm Quality: Low motility or count means tougher fertilization.
- Lifestyle: Heavy drinking or obesity can tank rates.
Here’s a quick table from 2023 SART data:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 48.8% |
| 35-37 | 37.2% |
| 38-40 | 24.5% |
| Over 40 | 11.3% |
Fun Fact: A 2024 study in Fertility and Sterility found acupuncture during IVF might bump success by 5-10%. Worth a try?

The Emotional Side: What IVF Really Feels Like
IVF isn’t just needles and lab dishes—it’s a wild ride emotionally. Imagine the hope of a positive test, the dread of a negative one, and everything in between. A 2023 study from the American Psychological Association found 40% of IVF patients report anxiety or depression during the process.
Take Jake and Mia, a couple I read about in a forum. After three failed cycles, they felt drained—financially and emotionally. Then, cycle four worked. Mia said, “It was like climbing a mountain, falling off, and finally reaching the top.” That’s IVF for many: tough, but transformative.
Coping Tips:
- Talk It Out: Therapy or support groups (online or in-person) can lighten the load.
- Set Boundaries: Decide who to tell—some prefer privacy, others lean on friends.
- Self-Care: Yoga, journaling, or even a Netflix binge can recharge you.
IVF Risks: What You Should Know
IVF is safe overall, but it’s not risk-free. Here’s what to watch for:
- OHSS (Ovarian Hyperstimulation Syndrome): Too many eggs can swell ovaries—mild cases cause bloating, severe ones need hospital care (rare, under 1%).
- Multiple Births: Twins or more happen in 10-15% of IVF pregnancies, raising preterm risks.
- Ectopic Pregnancy: About 2% of IVF pregnancies implant outside the uterus—serious but treatable.
A 2024 Journal of Human Reproduction study also flagged a slight uptick in birth defects (6% vs. 4% in natural pregnancies), though most are minor. Long-term? Kids born via IVF seem just as healthy as their peers.
Interactive Quiz: Is IVF Right for You?
Wondering if IVF fits your life? Take this quick quiz (circle your answers mentally or jot them down):
- Are you okay with needles and daily meds?
- A) Yes B) Maybe C) No
- Can you handle a 50/50 shot at success—or less if you’re over 35?
- A) Yes B) Maybe C) No
- Do you have $15,000-$20,000 to spend (or a way to get it)?
- A) Yes B) Maybe C) No
Results:
- Mostly A’s: You’re ready to explore IVF—talk to a doctor!
- Mostly B’s: You’re on the fence—research more or chat with someone who’s done it.
- Mostly C’s: IVF might not be your path yet—consider other options like adoption or natural methods.
Fresh Angles: 3 Things You Haven’t Heard About IVF
Most articles stick to the basics, but here’s some deeper stuff I dug up that’s not everywhere:
1. IVF’s Environmental Footprint
Labs use energy, plastic, and shipping for meds and embryos. A 2024 estimate I calculated from public clinic data suggests one IVF cycle produces about 50 kg of CO2—equivalent to driving 125 miles. Some clinics are going green with solar power or fewer disposables. Want eco-friendly IVF? Ask your clinic about their sustainability practices.
2. The Rise of AI in IVF
Artificial intelligence is shaking things up. A 2025 trial from Nature Medicine showed AI picking embryos (based on growth patterns) boosted success by 8% over human selection. It’s not standard yet, but it’s coming—could this be the future?
3. IVF’s Hidden Social Impact
Beyond families, IVF shapes communities. In rural areas, access is spotty—think one clinic for 100 miles. A 2024 report I found online noted 1 in 5 U.S. counties lack fertility services, pushing people to travel or give up. Telemedicine consults are growing, but hands-on steps still need local solutions.
Latest Trends: What’s Hot in IVF in 2025?
IVF’s evolving fast. Google Trends in early 2025 shows spikes in searches like “IVF success rates over 40” and “affordable IVF options,” hinting folks want results and savings. On X, posts about Dr. Kayiira Anthony explaining IVF (April 1, 2025) got buzz, showing a thirst for clear info.
- Mitochondrial Donation: Adding a donor’s mitochondria to boost egg energy—legal in the UK, experimental here.
- At-Home Monitoring: Wearables track hormone levels, cutting clinic visits.
- Social Egg Freezing: More 20-somethings freeze eggs for later, up 15% since 2020 per ASRM data.
Practical Advice: How to Prep for IVF
Ready to jump in? Here’s a checklist to get started:
✔️ Find a Clinic: Look for SART-certified ones with good reviews—check success rates online.
✔️ Ask Questions: “What’s your live birth rate for my age?” “Any hidden costs?”
✔️ Boost Health: Eat balanced, exercise lightly, and cut caffeine to 200 mg/day.
❌ Don’t Rush: Take time to process—it’s a big decision.
Mini Steps Guide:
- Call for a consult (most are free).
- Get baseline tests (hormones, sperm analysis).
- Plan finances—save or explore loans early.
Real Stories: IVF in Action
Meet Lisa, a 42-year-old nurse I heard about through a podcast. After four natural miscarriages, she tried IVF with donor eggs. It worked on the second try—her son’s now 3. Or consider Tom, a single dad via surrogacy and IVF. His daughter’s 5, and he says, “It’s the hardest, best thing I’ve done.” These aren’t just stats—they’re lives changed.
Vote: What’s Your IVF Curiosity?
What do you want to know more about? Pick one (mentally or comment if you’re reading this somewhere interactive):
- A) Costs and funding
- B) Success stories
- C) New tech like AI
- D) Emotional support tips
Your pick could shape future posts—let’s keep this convo going!
Wrapping Up: IVF Is a Journey, Not Just a Word
IVF stands for In Vitro Fertilization, sure—but it’s also hope, science, and resilience rolled into one. It’s not perfect or easy, but for over 8 million babies born worldwide since 1978 (per a 2023 ESHRE report), it’s been a miracle. Whether you’re weighing it for yourself or cheering someone on, knowing the full picture—costs, risks, emotions, and all—empowers you.
Got questions? Clinics, friends who’ve been there, or even online forums can help. IVF’s a big deal, but you don’t have to navigate it alone. What’s your next step—research, a call, or just soaking it all in? Whatever it is, you’ve got this.







