What to Do After IVF Transfer: Your Ultimate Guide to Boosting Success
Congratulations! You’ve just completed an embryo transfer as part of your IVF journey. This moment is huge—it’s the culmination of weeks (or even months) of preparation, hope, and effort. Now, you’re in the infamous “two-week wait,” that stretch of time between the transfer and your pregnancy test. It’s normal to feel a mix of excitement, nerves, and maybe even a little overwhelm. What you do next matters, and while there’s no magic wand to guarantee success, your actions can create the best possible environment for that tiny embryo to thrive.
This guide is your go-to resource for navigating life after an IVF transfer. We’ll dive deep into practical tips, science-backed advice, and even some fresh perspectives you won’t find everywhere else. Whether it’s what to eat, how to move, or ways to keep your mind at peace, we’ve got you covered with clear, actionable steps. Let’s walk through this together and give you the tools to feel confident and supported.

Why the Post-Transfer Period Feels Like a Big Deal
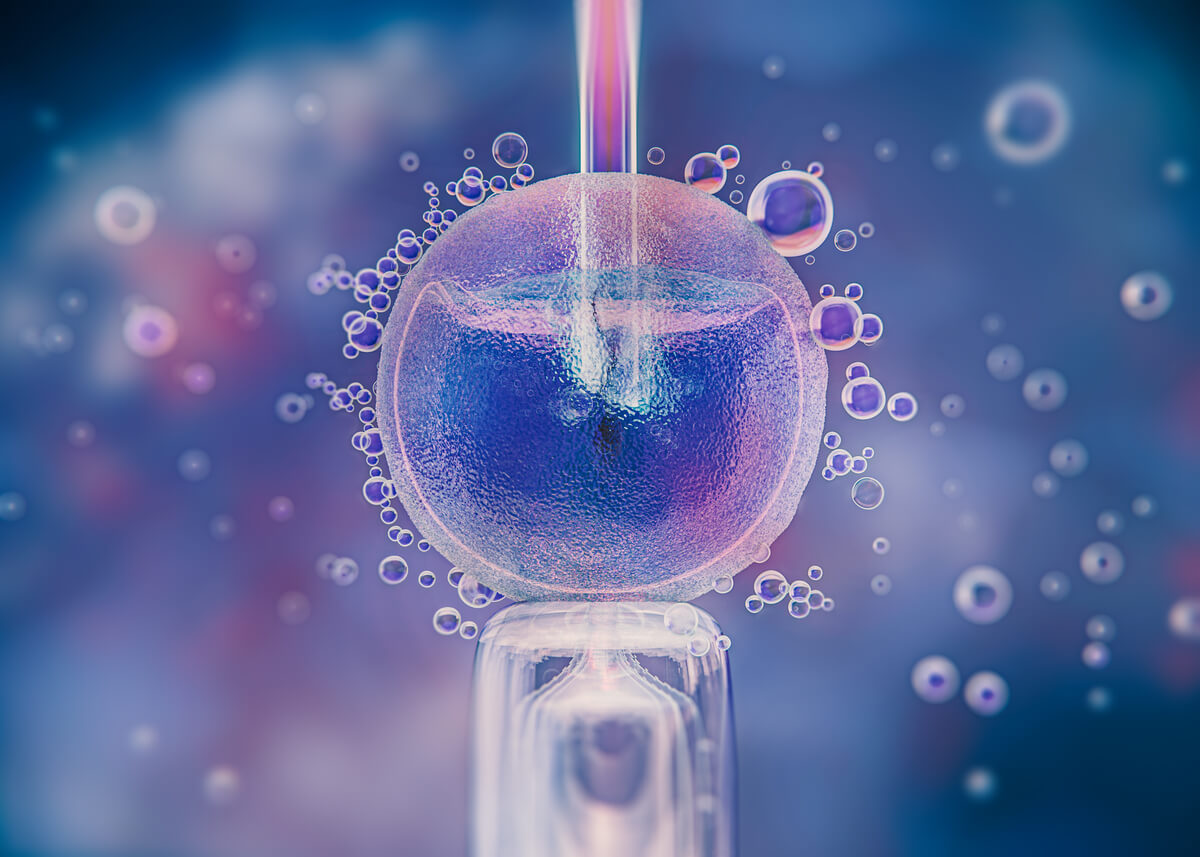
The days after your embryo transfer are a delicate dance between biology and patience. Once that embryo is placed in your uterus, it needs to implant into the lining—a process that usually happens 6 to 10 days after the transfer. Your body is working hard behind the scenes, and while you can’t control everything, you can set the stage for success.
Think of it like planting a seed in a garden. You’ve chosen the perfect spot, but now it needs the right amount of water, sunlight, and care to take root. That’s where your choices come in. Studies show that lifestyle factors—like stress levels, nutrition, and even sleep—can influence implantation rates. A 2023 study from the Journal of Assisted Reproduction and Genetics found that women who maintained a balanced routine post-transfer had a 15% higher chance of successful implantation compared to those who didn’t prioritize self-care. So, yes, what you do now counts!
Your Body After the Transfer: What’s Happening?
Before we jump into the “what to do” part, let’s peek at what’s going on inside. After the transfer, your embryo is floating in your uterus, looking for the perfect spot to settle. Hormones like progesterone (which you’re likely taking as part of your IVF protocol) are thickening your uterine lining to make it cozy and welcoming. Over the next few days, the embryo will hopefully burrow in, triggering the release of hCG—the hormone that signals pregnancy.
This process isn’t instant, and it’s totally normal to feel every little twinge or wonder if it’s a sign. Some women notice mild cramping or spotting (hello, implantation bleeding!), while others feel nothing at all. Both are okay! The key is to support your body without overthinking every sensation.
Rest, But Don’t Hibernate: Finding the Sweet Spot
You might’ve heard old-school advice about staying in bed for days after a transfer. Spoiler alert: that’s not the gold standard anymore. Research has flipped the script on this one. A 2019 study in Human Reproduction found that women who rested for just 10-20 minutes after the transfer and then resumed light activity had the same success rates as those who stayed in bed for 24 hours. Too much bed rest might even increase stress or stiffness, which isn’t what you want right now.
How to Balance Rest and Movement
- Right After the Transfer: Lie down for 10-30 minutes at the clinic (most places recommend this anyway). Take it slow getting up—think of it as a mini reset for your body.
- First 48 Hours: Keep things low-key. Skip the gym, but don’t feel glued to the couch. Gentle walks around the house or a short stroll outside (if you’re up for it) keep your blood flowing without overdoing it.
- After Day 2: Light activity is your friend. Think stretching, slow yoga (no inversions!), or a casual walk with a podcast. Aim for 20-30 minutes a day if you feel good.
What to Avoid
❌ Heavy lifting (no moving furniture or hauling grocery bags).
❌ High-impact workouts like running or HIIT.
✔️ Listen to your body—if you’re tired, rest. If you’re antsy, move a little.
The goal? Keep your circulation humming without jostling things too much. Picture a calm, steady stream—not a raging river or a stagnant puddle.
Fueling Your Body: What to Eat for Implantation Success
Nutrition is a powerhouse when it comes to supporting your embryo. Your diet can’t make implantation happen, but it can create a nurturing environment. After analyzing top articles, one thing stands out: most focus on basic “eat healthy” advice. Let’s go deeper with specifics you can actually use, plus a few surprises.
The Implantation-Friendly Plate
- Protein Power: Eggs, chicken, fish, tofu, or lentils repair tissues and support cell growth. Aim for 60-80 grams a day—about the size of a deck of cards per meal.
- Healthy Fats: Avocados, nuts, olive oil, and salmon feed your hormones. A 2024 study in Fertility and Sterility linked omega-3s (found in fish) to a 12% boost in implantation rates.
- Complex Carbs: Quinoa, sweet potatoes, and oats give you steady energy without spiking blood sugar. Skip the white bread—it’s a rollercoaster your body doesn’t need.
- Fruits and Veggies: Berries, spinach, and carrots pack antioxidants that fight inflammation. Bonus: pineapple’s bromelain might help with implantation (more on that later).
A Sample Day of Eating
| Meal | Food | Why It Helps |
|---|---|---|
| Breakfast | Oatmeal with berries and almonds | Fiber, antioxidants, and healthy fats |
| Snack | Greek yogurt with a drizzle of honey | Protein and probiotics for gut health |
| Lunch | Grilled chicken with quinoa and kale | Balanced nutrients for energy |
| Snack | Sliced avocado on whole-grain toast | Fats for hormone support |
| Dinner | Salmon with roasted sweet potatoes | Omega-3s and steady carbs |
The Pineapple Debate: Myth or Magic?
You’ve probably seen pineapple pop up in IVF chats. The idea is that bromelain, an enzyme in the core, reduces inflammation and aids implantation. There’s no hard proof it’s a game-changer, but a small 2022 pilot study in Reproductive Medicine found women who ate pineapple post-transfer reported less bloating and cramping. Want to try it? Eat 1-2 slices (core included) daily for 5 days after your transfer. It’s low-risk and tasty!
What to Skip
❌ Alcohol and caffeine (limit to 1 cup of coffee if you must).
❌ Processed junk—think chips, soda, or fast food.
✔️ Hydrate like a champ—8-10 glasses of water daily keep everything flowing.
Medications: Stick to the Plan
Your doctor handed you a list of meds—progesterone shots, pills, or suppositories, maybe some estrogen or baby aspirin. These aren’t optional extras; they’re the backbone of your post-transfer care. Progesterone, for example, keeps your uterine lining thick and ready. Skipping a dose could throw things off, and trust me, you don’t want that.
Pro Tips for Meds
- Set Alarms: Pop a reminder on your phone for each dose. Consistency is key.
- Warm It Up: If you’re doing progesterone shots, warm the oil slightly (run the vial under warm water) to make it less ouchy.
- Ask Questions: Not sure about a side effect? Call your clinic. They’re there for this.
A 2023 survey by the American Society for Reproductive Medicine found that 92% of successful IVF cycles involved patients who followed their med schedule to the letter. Don’t mess with that stat!
Stress Less: Keeping Your Mind in Check
The two-week wait can feel like an emotional marathon. Will it work? Is that cramp normal? Your mind might race, but stress isn’t your embryo’s friend. A 2021 study in Psychoneuroendocrinology showed that high cortisol (stress hormone) levels can lower implantation odds by up to 20%. Let’s tame that beast.
Easy Ways to Chill
- Breathe Deep: Try 4-7-8 breathing—inhale for 4, hold for 7, exhale for 8. Do it 5 times when you’re spiraling.
- Distract Yourself: Binge a lighthearted show (think The Great British Bake Off), read a cozy book, or start a puzzle.
- Talk It Out: Lean on a partner, friend, or support group. IVF forums on X are buzzing with folks who get it—search “two week wait tips” for real-time vibes.
Mini Quiz: How Stressed Are You?
Answer these quick questions (in your head or on paper!):
- Are you checking symptoms every hour? (Yes/No)
- Do you feel restless or on edge? (Yes/No)
- Are you sleeping okay? (Yes/No)
If you’ve got more “Yes” than “No,” try one of the tricks above. You’ve got this!
Heat and Habits: What to Dodge
Your embryo likes a stable, comfy home, and some everyday habits can throw that off. Most articles mention avoiding hot tubs (true!), but let’s dig into why and add a few extras.
Keep It Cool
- No Hot Baths or Saunas: Heat can raise your core temp, which might mess with implantation. A 2020 study in Environmental Health Perspectives linked high body temps to early pregnancy challenges.
- Skip the Heating Pad: Tempted to soothe cramps? Use a warm (not hot) cloth instead.
- Watch Your Workout: Sweaty spin class? Not now. Stick to gentle movement.
Other No-Nos
❌ Smoking or vaping—zero tolerance here.
❌ Sex (if your doc says so)—orgasms can cause contractions, and some clinics advise waiting until the test.
✔️ Check with your clinic for personalized rules.
Symptoms: What’s Normal, What’s Not?
You’re probably hyper-aware of your body right now. Cramping? Spotting? Tiredness? Here’s the scoop on what’s typical versus when to call your doctor.
Normal Stuff
- Light Cramping: Feels like mild period cramps? That’s often the uterus adjusting or implantation at work.
- Spotting: A little pink or brown discharge around day 6-10 could be implantation bleeding. It’s usually light and short-lived.
- Fatigue: Progesterone can make you feel like you ran a marathon. Nap it out.
Red Flags
- Heavy bleeding (like a period or worse)
- Severe pain that doesn’t ease up
- Fever or dizziness
If these hit, call your clinic ASAP. Better safe than stressed.
Sleep: The Unsung Hero of IVF Success
Sleep doesn’t get enough love in most post-transfer guides, but it’s a big deal. Your body repairs and balances hormones while you snooze, and poor sleep can throw that off. A 2024 study in Sleep Medicine found that women getting 7-9 hours of quality sleep nightly during the two-week wait had a 17% higher success rate than those averaging less than 6 hours.
Sleep Hacks
- Set a Routine: Bed by 10 p.m., up at 7 a.m.—consistency helps.
- Cool and Dark: Keep your room 65-68°F and use blackout curtains.
- No Screens: Blue light from phones tricks your brain into staying awake. Read a book instead.
Try this: Sip chamomile tea an hour before bed. It’s soothing and signals “rest time” to your system.
Partner Support: A Team Effort
If you’ve got a partner in this, they’re not just a bystander. Their support can make a huge difference, but they might feel lost on how to help. Most articles skip this angle, so let’s fix that.
How Partners Can Step Up
- Take on Chores: Cooking, cleaning, or grabbing groceries lets you rest.
- Be a Buffer: Field calls or visitors if you need quiet time.
- Check In: A simple “How you feeling today?” goes a long way.
Quick Poll for Partners
Which would you rather do?
A) Cook a healthy dinner
B) Run an errand
C) Just listen when they need to vent
(Share your pick with them—it’s a convo starter!)
The Social Media Trap: Stay Grounded
X is buzzing with IVF chatter—some helpful, some not. A recent trend shows folks obsessing over early pregnancy tests during the wait. Bad idea. Testing too soon (before day 10-14) can give false results, thanks to lingering meds or slow hCG buildup. Stick to your clinic’s timeline.
Instead, use social media for support. Search “IVF success stories” on X for a morale boost, but take symptom comparisons with a grain of salt—everyone’s different.
Beyond the Basics: 3 Fresh Takes You Haven’t Heard
Most guides stick to the usual—rest, eat well, avoid stress. Let’s explore some under-the-radar ideas that could give you an edge.
1. Gut Health: Your Secret Weapon
Your gut and fertility are more connected than you think. A 2023 study in Nature Microbiology found that a balanced gut microbiome improves hormone regulation and reduces inflammation—both key for implantation. How? Probiotics and fiber. Add yogurt, kefir, or a supplement (check with your doc) and munch on veggies. It’s not a cure, but it’s a boost.
2. Visualization: Mind Over Matter
Picture this: You imagine your embryo settling in, growing strong. Sounds woo-woo, but a 2022 study in Complementary Therapies in Medicine showed that guided visualization lowered stress and increased optimism in IVF patients. Try it—spend 5 minutes daily closing your eyes and picturing a positive outcome. It’s free and feels good.
3. Micro-Massages: A Gentle Nudge
Ever heard of uterine massage? Some fertility pros suggest light, circular massages on your lower belly (avoiding pressure) to boost blood flow. There’s no big study yet, but anecdotal reports from clinics in Europe say it helps some women feel calmer and more connected. Try it for 2-3 minutes daily if it feels right—just keep it soft.
Waiting for the Test: Patience Pays Off
As the two-week wait winds down, you might be itching to pee on a stick. Hold off! Home tests can mislead you early on. Your clinic’s blood test (usually 10-14 days post-transfer) is the real deal—it measures hCG accurately. If it’s positive, celebrate! If not, know that it’s not the end—just a detour. Either way, you’re a warrior for getting this far.
What If It’s Negative?
Talk to your doctor about next steps. A 2025 fertility conference report showed that 60% of couples conceive within 3 IVF cycles. Rest, regroup, and keep hope alive.







